Have chronic pain? Changing your beliefs about it can make you feel better
- Chronic pain is often attributed to tissue damage, but it is often due to reversible changes in the brain and peripheral nerves.
- False beliefs about the causes of chronic pain can make you feel worse.
- A psychological treatment that changes patients’ beliefs about the causes of their pain can reduce pain intensity.
Pain typically occurs as a result of illness or injury, and usually diminishes and then disappears with recovery. In some people, however, pain can occur in the absence of any injury and despite medication or treatment. When it persists for longer than three months, it is defined as chronic pain.
Mind-body problem
Patients suffering from chronic pain often hold the belief that their pain is due to tissue damage from a bulging disc, osteoarthritis, or some other ailment. In many cases, however, this is not the cause of the symptoms. Instead, the pain is driven primarily by neuroplastic processes in the brain and peripheral nerves. Furthermore, the false belief can actually exacerbate the pain by leading to fear avoidance behavior, whereby the patient avoids physical activity that they think will worsen the pain or cause re-injury.
New research published in the journal JAMA Open Network now shows that a psychological treatment that helps patients reattribute their pain to reversible neural pathways can significantly reduce the intensity of the pain they feel.
Pain reprocessing therapy
Yoni Ashar of the University of Boulder in Colorado and his colleagues recently developed pain reprocessing therapy (PRT), a psychological treatment that aims to break the cycle of chronic pain by teaching patients to interpret and respond to bodily signals differently. Earlier this year, they published the results of a small randomized clinical trial of 151 patients with low to moderate back pain, which showed that those patients who received the therapy were free from pain after treatment compared to those in the control groups.
Their latest study aimed to gain a better understanding of the psychological mechanisms underlying PRT. They asked 135 of the original participants to self-report the causes of their pain, by means of questionnaires, completed before and after they received the treatment or placebo. The participants’ pre-treatment responses varied widely, and so the researchers grouped responses into 11 categories, the most common being activity (25%) and injury (19%). A small minority of the responses (less than 10%) were categorized as being mind- or brain-related. (See figure.)
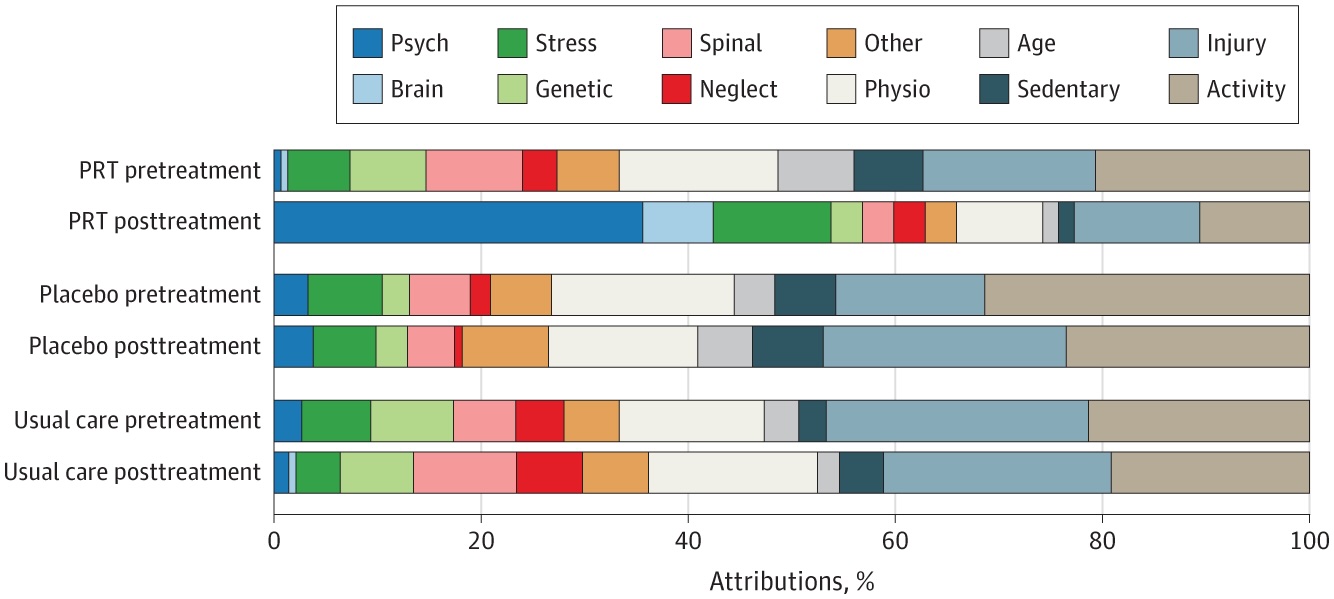
PRT, however, significantly increased the number of post-treatment responses attributing the pain to mind- or brain-related causes. Notably, the word “anxiety” appeared far more frequently in the self-reports of those who had received the psychological treatments. These patients also introduced other emotion-related words, such as “fear” and “feelings,” and neurobiological terms, such as “neural pathways,” while decreasing their use of words related to physical attributions, like “activity,” “weight,” and “sport.”
The increases in what the researchers call “mind-brain attribution scores” were associated with decreased pain intensity and fewer fear avoidance behaviors in some of the patients. Still, others changed their attribution scores dramatically but saw no change in the pain they experienced. Nevertheless, the results suggest that using simple language to help patients reattribute pain from the body to the brain could be a useful approach to treatment.