Always tired? Your immune system may be overactive.

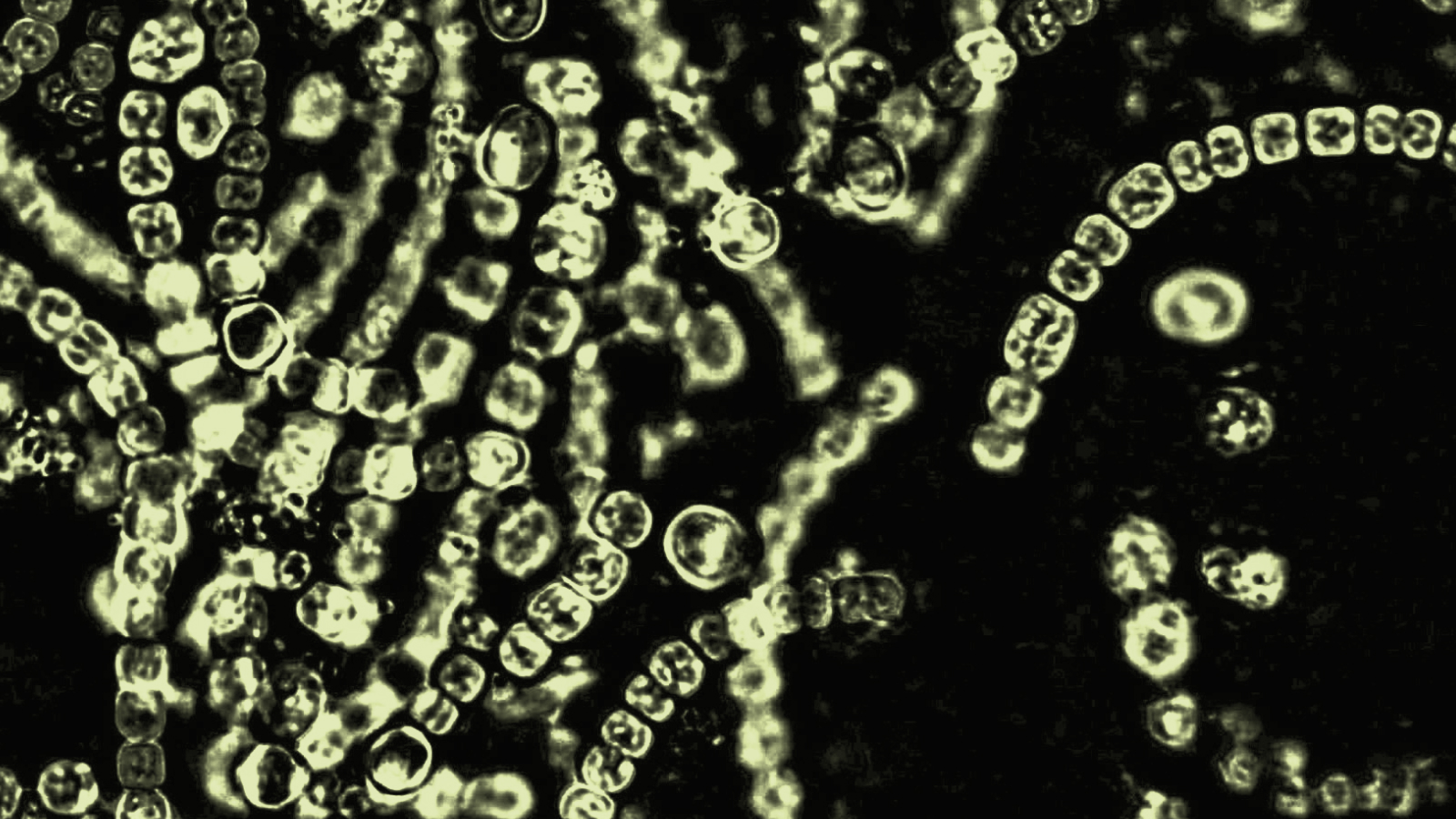
Pixabay
- Chronic fatigue syndrome affects millions of people worldwide, but scientists still aren’t quite sure what causes it.
- A new study tracked people suffering from Hepatitis C (HCV) as they underwent a treatment course.
- The results showed that people with overactive immune responses developed chronic fatigue months following the treatment, and that the fatigue persisted even after their immune responses returned to normal.
A new study builds upon previous research showing that an overactive immune system might be a key cause of chronic fatigue syndrome.
Chronic fatigue syndrome (CFS), also called myalgic encephalomyelitis (ME), is a debilitating condition that leaves people feeling always tired and mentally foggy. Worse, sleep doesn’t really help to alleviate the symptoms of CFS, which affects some 17 million people worldwide.
The causes of CFS remain unknown. In recent years, however, research has suggested that an overactive immune system might be to blame. But that hypothesis has been difficult to study because it’s impossible to tell who’s going to contract a virus, and researchers need to examine physiological conditions before, during and after an immune response occurs.
A recent study — it was published in the journal Psychoneuroendocrinologyon December 17 — used a novel approach to get around that problem. Researchers at King’s College London recruited 55 patients with chronic Hepatitis C (HCV) and gave them a six- to 12-month course of a drug called Interferon alpha, a common treatment for HCV. Then, the team tracked the participants as they recovered.
Six months after the treatment ended, 18 participants were more fatigued than before the course began. Before treatment, these participants showed relatively high levels of a protein linked to inflammation, called IL10, in their blood. These levels, including levels of another protein linked to inflammation, only increased after four weeks of treatment, reaching levels twice as high as people who recovered without chronic fatigue.
However, six months after the treatment, the 18 fatigued participants also showed immune-response levels that were no different from participants who hadn’t developed post-treatment fatigue. What’s more, the researchers took samples of these inflammation proteins from all the participants and compared them to those of 57 separate healthy participants who didn’t have HCV or undergo the treatment. The results showed no difference between the two sets.
A possible cause
One theory is that a hyperactive immune response triggers CFS. Still, that doesn’t explain exactly what role the immune system plays in the later stages of the condition, considering there appear to be no abnormal immune responses once symptoms emerge.
“In conclusion, findings from this study support the hypothesis that abnormal immune mechanisms are important in CFS, but only early in the course of the illness, around the time of the trigger, rather than when the syndrome is established,” the authors wrote. “Moreover, our study confirms the importance of the acute fatigue response to the trigger, rather than of the recovery period preceding the illness.”
The findings could give researchers “some clue down the line” as to the exact causes and possible treatments for CFS, Michael Sharpe, a professor of psychological medicine at the University of Oxford, told The Guardian.
“If the thing is triggered by an abnormal or excessive immune response, if we could find a way to reduce that immune response, we might stop incident cases,” Sharpe said.