Major Hospitals are Offering Alternative Therapies. Is This Medicine?

You check in at the hospital for chronic back pain. The doctor asks you to follow her past the MRI machines and operating room to a recently converted yoga studio. An unrolled mat awaits. En route you peek your head into an adjacent treatment room to watch an acupuncturist needling a patient. Rows of IV drips and homeopathic remedies line the shelves.
This not uncommon scene plays out in many small centers across the nation. Yet as Stat News reports, some of the country’s top hospitals and institutions are offering the same modalities, to mixed reviews. Staff and administrators claim to be listening to patient desires. Critics state this is not good medicine.
Part of the problem is that the numerous therapeutic modalities existing outside of the purview of ‘Western’ medicine are lumped together into the ambiguous ‘alternative therapies.’ Yoga and meditation, for example, have been clinically studied over the last few decades, showing promising results for pain relief, anxiety, and cognitive functioning. Homeopathy and ‘energy healing,’ however, have at best been shown to be no better than the placebo response.
When dealing with the common cold, using an ineffective or unproven therapy such as a homeopathic proving is largely benign—the placebo response might prove helpful in such circumstances. But this trend is more insidious, Stat reports. The “spa-like wellness centers” are branding their own forms of mysticism, offering questionable treatments for cancer, heart disease, and chronic pain.
Duke even markets a pediatric program that suggests on its website that alternative medicine, including “detoxification programs” and “botanical medicines,” can help children with conditions ranging from autism to asthma to ADHD.
Separating wheat from chaff is challenging in the modern medical environment. Our emotions and perceptions really do play a role in healing, a major criticism of the ‘cold mechanisms’ of Western medicine. One 1984 study found that the view from your hospital room influences healing time; more recent research suggests that hospital gardens are effective in speeding recovery. This makes sense as our environment always affects our nervous and immune systems. Being in a calm, peaceful space or gazing at a mountain lifts our mood, which aids healing.
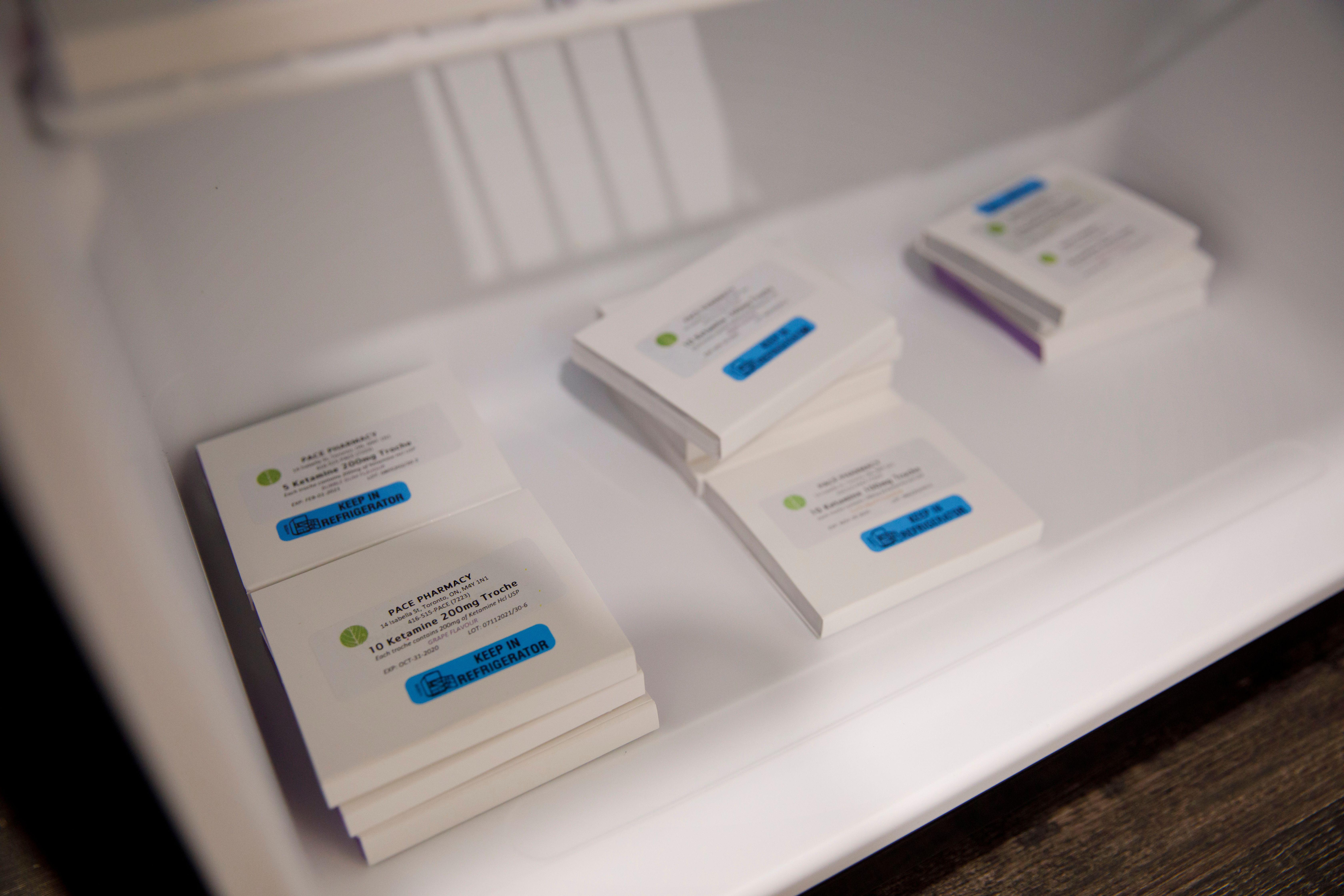
The trend toward offering mineral and vitamin IV drips, by contrast, appears to be a money grab. Excess vitamins have detrimental effects. The notion that more is better is provably false. One IV drip purporting to “attack and shorten illness” features high doses of Vitamin C, zinc, and lysine, all of which create GI problems at high doses. It costs $175 an hour. For ten dollars less you can get a “fat burner” containing L-carnitine. Side effects of this amino acid include diarrhea, seizures, and vomiting, as well as causing your breath, sweat, and urine to have a fishy odor.
Not everyone experiences such side effects, nor are elevated doses of vitamins and minerals for short durations necessary harmful. They’re even therapeutic under certain circumstances. Ordering a boost without credible supervision because you read a wellness blog claiming it helps shed visceral fat, though, does not honor the Hippocratic oath. It merely drains your wallet while putting you at risk of potential side effects.
Acupuncture is another common menu item. The system is based on unproven meridian channels and roughly four hundred points along the body. Research on its efficacy is mixed, with many studies finding it no more effective than placebo. But as interest grows, more research is being conducted. A recent study published in Brain found traditional points effective in treating long-term pain associated with carpal tunnel syndrome.
Some research states that adenosine might be the therapeutic mechanism behind acupuncture. Studies investigating electroacupuncutre, like the one published in Brain, are different from the style originating in Traditional Chinese Medicine, as an electric current is passed between pairs of needles. Add to this the time spent relaxing on a table listening to ambient music and it’s challenging to know what exact mechanisms are at play. That said, if a technique is shown to work, hospitals and clinics have a duty to offer it to patients. It should not be discredited if there is positive evidence in certain situations.
Perhaps the biggest challenge in this whole movement is egos. Doctors, nurses, researchers, and clinicians stand their ground. With insurance in disarray even major institutions are struggling to find revenue streams. One clinician at UCLA, also a licensed acupuncturist that formerly worked in integrative medicine at Cedars, told me,
The world of Western medicine is extremely territorial. Physicians, nursing, all positions in the paradigm fight vigorously to hold their ground and protect scope of practice. It’s very difficult to generate revenue for an IMG [integrative medical group] in the hospital setting, which is why a lot of them fail. Billing proves problematic.
Hopefully one day our notion of medicine will expand beyond invasive surgical techniques and pharmaceuticals and embrace modalities that are less expensive with fewer side effects. We should welcome major institutions integrating such therapies into their programs.
Yet when this movement is fueled by popular demand and not credible science we run into the same problems patients encounter when enduring pharmaceutical cocktails, overpriced treatments, and rushed doctors. Since before the days of Hippocrates medicine has been as much a work of art as science. Trendy vitamin drips and energy healing might bring in revenue but do not honor the oath each professional is bound to. Throw down a meditation cushion to help forge a mind-body connection, but leave homeopathic bee venom behind.
—
Derek’s next book, Whole Motion: Training Your Brain and Body For Optimal Health, will be published on 7/4/17 by Carrel/Skyhorse Publishing. He is based in Los Angeles. Stay in touch on Facebook and Twitter.