Antimicrobial resistance is a growing threat to good health and well-being

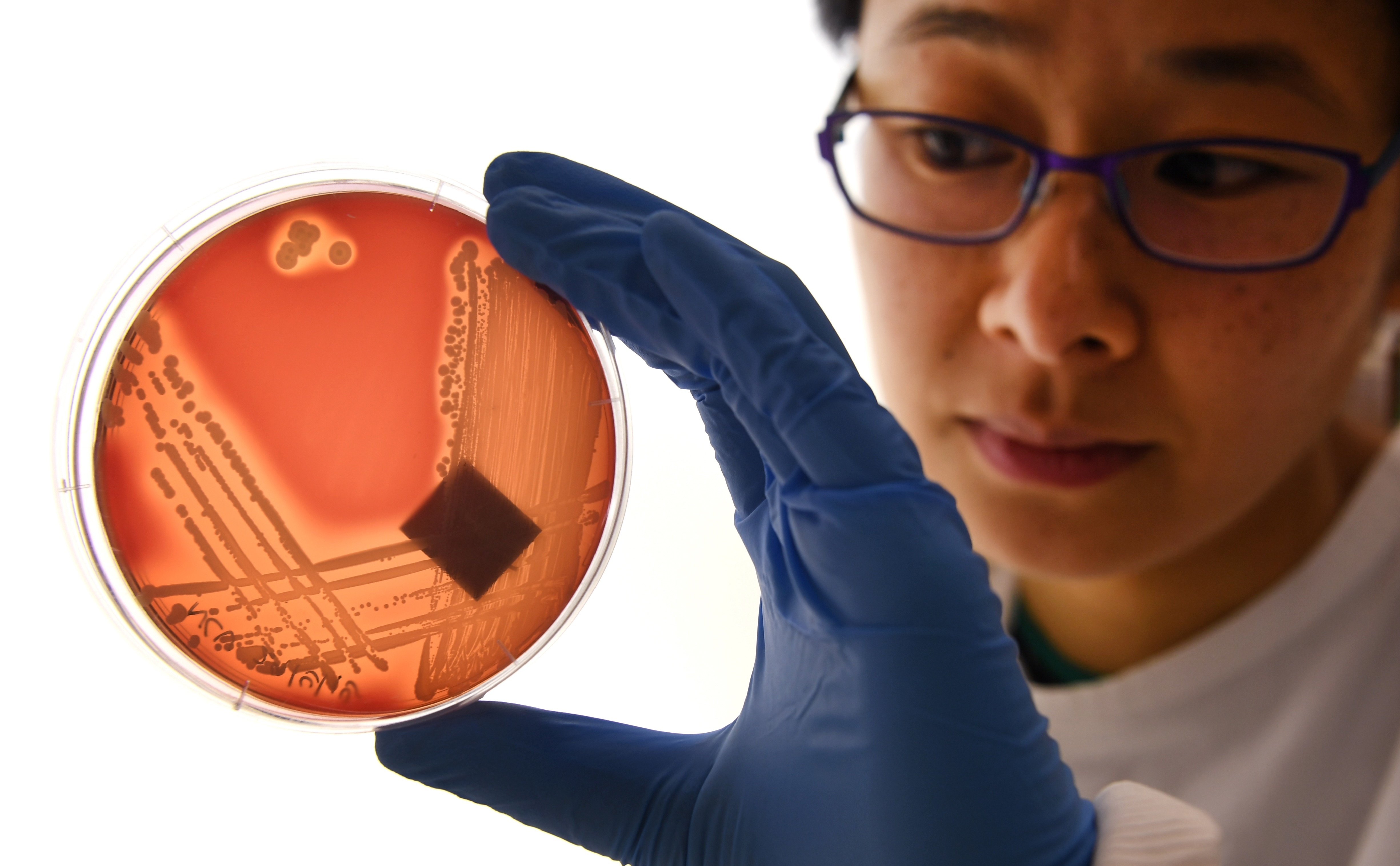
Image courtesy of Pfizer.
- Antimicrobial-resistant pathogens are one of the largest threats to global health today.
- As we get older, our immune systems age, increasing our risk of life threatening infections. Without reliable antibiotics, life expectancy could decline for the first time in modern history.
- If antibiotics become ineffective, common infections could result in hospitalization or even death. Life-saving interventions like cancer treatments and organ transplantation would become more difficult, more often resulting in death. Routine procedures would become hard to perform.
- Without intervention, resistant pathogens could result in 10 million annual deaths by 2050.
- By taking a multi-faceted approach—inclusive of adherence to good stewardship, surveillance and responsible manufacturing practices, as well as an emphasis on prevention and treatment—companies like Pfizer are fighting to help curb the spread.
Antibiotics have revolutionized healthcare.
With the advent of modern medicine, life threatening diseases such as smallpox, pertussis (whooping cough), tetanus (lockjaw) and measles have essentially been eradicated. More importantly, complicated procedures that increase our risk of infections—including plastic surgery, joint replacement, cancer treatments, and organ transplant, among others—have become routine because any resulting infection can be treated effectively.
But modern medicine depends on antibiotics to treat and cure many kinds of infections—infections that could impact anyone from the premature baby to the elderly. Unfortunately, antimicrobial resistance (AMR) has made some infections impossible and others increasingly difficult to treat, threatening the progress we have worked so hard to achieve.
AMR causes 700,000 deaths annually across the globe, a number projected to skyrocket to 10 million by 2050 without intervention.
What is antimicrobial resistance?
Antimicrobial drugs target the microorganisms that cause infection, such as bacteria, viruses, fungi, and parasites, and either kills them or inhibits their growth.
Anytime an antibiotic is used, either appropriately or inappropriately, the 30 trillion or more bacteria that live in or on our bodies undergo selective pressure to become resistant. Any that are sensitive to the antibiotic are killed, while those that remain are resistant or immune from the effects of that antibiotic. This is called AMR. Once a bacterial pathogen has reached a state of resistance to several types of antibiotics, it is colloquially referred to as a “superbug.”
The consequences of AMR can be stated simply: Commonly used antibiotics are rendered ineffective against that pathogen. If an infection caused by resistant bacteria is treated by that antibiotic, the bacteria are unaffected, resulting in disease persistence, worsening of the infection and/or even death. Treatments for both minor and serious infections are compromised, surgeries and other routine procedures become riskier, and the treatment of diseases like pneumonia and tuberculosis becomes very complicated. For example, according to the World Health Organization, resistance in Klebsiella pneumoniae—a common intestinal bacterium that is a major cause of hospital-acquired infections, bloodstream infections, and infections in newborns and intensive-care unit patients—has spread to all regions of the world. In some countries, because of resistance, carbapenem antibiotics (often the “last resort” treatments) do not work in more than half of people treated for these types of infections. This results in prolonged hospitalization, increased medical costs and higher rates of death for infections that were easily treated only a few years ago.
“What’s more, AMR is a truly global issue—it can affect anyone, of any age, in any country,” Jill Inverso, Pfizer’s Vice President of Global Medical Affairs and Anti-Infectives, told Big Think.
AMR causes 700,000 deaths annually across the globe, a number projected to skyrocket to 10 million by 2050 without intervention. The rise of resistant pathogens is causing many countries to accrue significantly higher healthcare costs due to longer duration of illness, additional tests, and the need for different medicines to treat patients.
And these costs add up. The World Bank Group estimates that AMR could reduce annual global gross domestic product from 1.1–3.8 percent depending on severity, with up to $10.8 trillion in additional health expenditures.
At Pfizer, we take this growing threat very seriously and are driven by our desire to protect global public health and address the medical needs of people suffering from infectious diseases.
Giving antimicrobial resistance a helping hand
The development of bacterial resistance to antibiotics is a natural process. Unlike almost every other class of drugs, antibiotics drive their own obsolescence by selecting antibiotic-resistant bacteria, even when used appropriately according to guidelines. When this happens, resistant bacteria survive and continue to multiply, causing the infection to worsen. These resistant bacteria can then also spread to other patients, causing new infections with these bacteria that are difficult to treat.
Overuse and misuse of antibiotics accelerates this process without providing any benefit to the patient. This happens when patients take a drug without need, do not finish their dose or stop taking the medication mid-course; it could also happen when a drug is either overprescribed or prescribed for the wrong duration/type of illness. All of these misuses create environments in which pathogens are exposed to drugs more often, allowing them to acclimate and breed resistance without any benefit to the patient.
Hence, antibiotics must be used wisely and sparingly.
Fighting the resistance
WHO calls AMR an “increasingly serious threat to global public health” and one that “requires action across all government sectors and society.” Its widespread growth is threatening the United Nations General Assembly’s Sustainable Development Goal of Good Health and Well-Being.
Companies like Pfizer are heavily committed to the fight against AMR, taking action across a variety of areas such as surveillance, stewardship, and prevention and treatment.
On the surveillance front, Pfizer is proud to sponsor one of the largest AMR surveillance programs in the world, the Antimicrobial Testing Leadership and Surveillance (or ATLAS). ATLAS monitors real-time changes in bacterial resistance and tracks these trends in real-time. Gathering information from more than 760 hospitals across 73 countries in many underserved areas, ATLAS has generated 14 years of continuous global data on bacteria. Researchers and healthcare professionals can access ATLAS’s data—free of charge—to study resistance trends, even in emerging market countries like Africa, Asia, and Latin America.
“At Pfizer, we take this growing threat very seriously,” Inverso added, “and are driven by our desire to protect global public health and address the medical needs of people suffering from infectious diseases.”
Pfizer also encourages good stewardship practices and supports education and training programs to help ensure patients receive the correct antibiotic only if needed, at the right dose and for the right duration.
“We believe that everybody can play a part in AMR stewardship by not taking an antibiotic unless provided by a healthcare professional, sticking to antibiotic regimens when prescribed, and keeping their vaccinations up to date,” said Inverso. She added, “Vaccines are administered to help prevent infections from happening in the first place, thereby reducing the need for antibiotic usage that can lead to the development of resistance.”
To date, several studies have demonstrated the beneficial role vaccines play in the reduction of AMR, such as reducing the use of antibiotics by preventing bacterial infections which may, in turn, prevent antimicrobial resistant infections from developing. Pfizer is committed to continue the development of new, innovative vaccines to help prevent infectious diseases globally.
We believe that everybody can play a part in AMR stewardship by not taking an antibiotic unless provided by a healthcare professional, sticking to antibiotic regimens when prescribed, and keeping their vaccinations up to date.
Given this, we should ask ourselves the following:
- Have I ever not finished an antibiotic given to me by my doctor?
- Have I ever used an antibiotic given to someone else?
- Am I up-to-date on my vaccinations that prevent infections that would need antibiotics?
- Have I ever demanded an antibiotic for myself or a child that the doctor thought was caused by a virus?
- Have I ever saved antibiotics given to me for one infection and used it at a different time?
The key takeaway? AMR is a pervasive, growing threat that cannot be tamed without the collective efforts of government, industry, health systems, society and others. Working together, we may have a fighting chance.