Maia Szalavitz: Well, I think like in terms of—seeing famous people that we love die from drugs should make us question why we so stigmatize and attack people with addictions. I mean some of our most beloved artists, musicians, writers have been addicted. I mean I find it kind of interesting that we don't see addiction as a "white problem" when you have like William Burroughs and Lou Reed and Kurt Cobain—and I could list 20 other heroin addicted rock stars. So, this is a condition that can affect not just anybody, but people who are in some sort of emotional pain. Addiction kicks people who are already down. And it doesn't look like celebrities should be that kind of person. But I think that a lot of the drive and the grit and the, you know, what you need in order to achieve great success is also a risk for addiction. Because in order to be a successful rock star you have to process despite rejection a lot and you need to be able to just keep going and keep going. And if that kind of drive and passion gets focused on a drug it is particularly destructive.
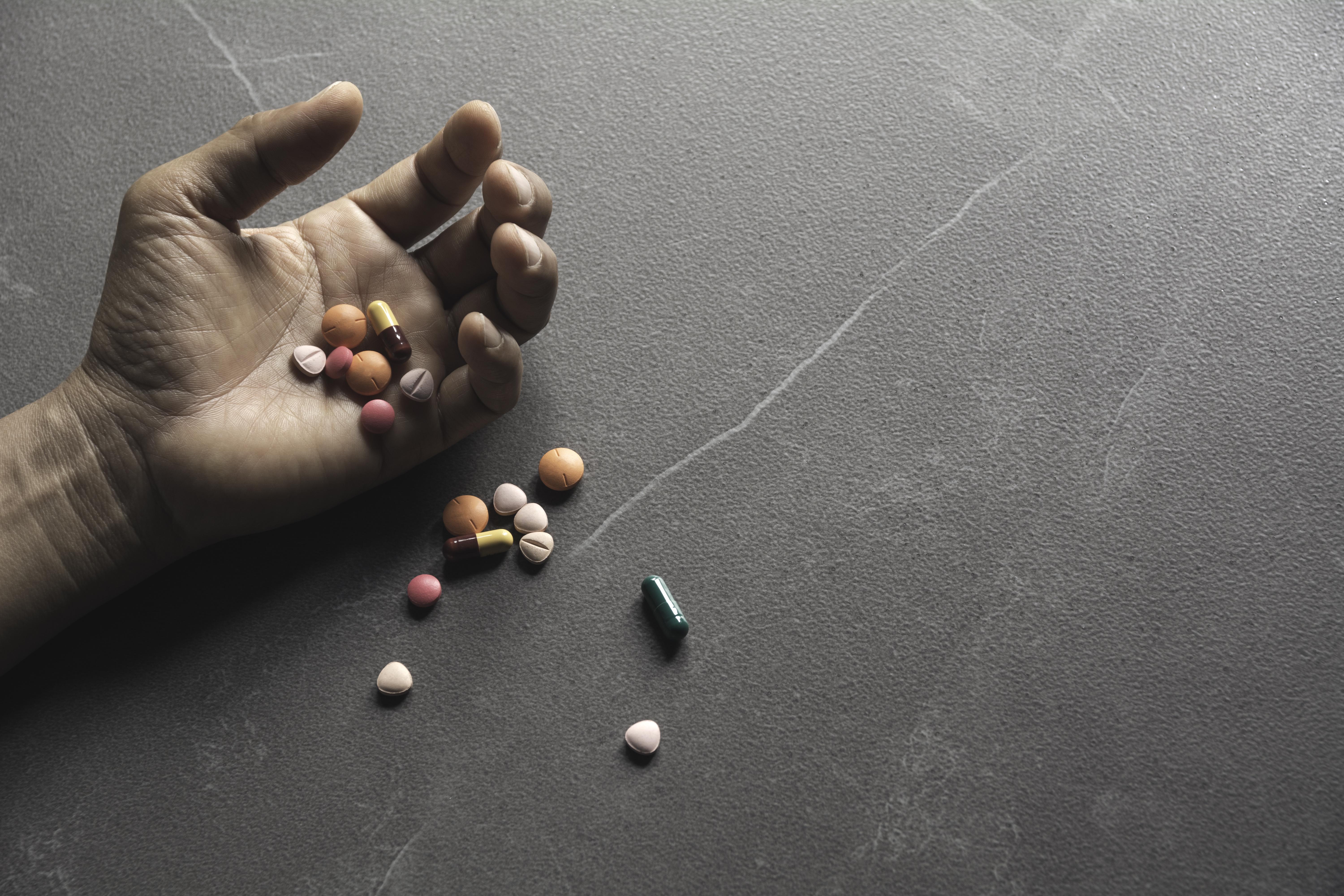
So, I think in order to help deal with opioid addiction, for one we need to have naloxone in every first aid kit. There is absolutely no reason why people who are surrounded by other people should ever die of an overdose. If you are injecting and other people are there—which is the case 50 to 60 percent of the time—naloxone should be there. And this is not going to encourage more drug use, because it's an awful experience to get awakened with naloxone, but it will save lives. And so that's one way we can turn the tide on this. The other way that I think we can turn the tide on opioid addiction is we really need to provide greater access to drugs like methadone and Suboxone, which is also called buprenorphine.
Those two drugs taken indefinitely, i.e. potentially for life, are the only thing that cut the death rate by 50 percent. And if we really want to solve this problem we could get rid of half of it if we could enroll many more people in these maintenance programs. Now there's a lot of the barriers to that. One is that we only allow doctors prescribing buprenorphine to see a hundred patients—now they just raised it to 200—this is ridiculous. They can prescribe opioids for pain to 10,000 patients but you can only prescribe for addiction to a hundred patients? This is really silly. We also have this idea that you can't provide these medications without also providing counseling. And we don't to do that for any other medical service. We don't say, "You can only get your insulin if you do X counseling on diet," or whatever. We realize that people need the tools to stay alive regardless of if they are improving as quickly as we would like them to do. And forced counseling doesn't actually help anyway. So what we should do is we should have different thresholds for treatment. So with buprenorphine some people may just want to show up and get a dose, and that's it. And that will work as sheer harm reduction. That should be available in emergency rooms.
You need to register people so that you don't end up with people getting multiple doses, and you need to be a little more careful with methadone than with buprenorphine because there is a big overdose risk for patients who are naïve to methadone, and it's a difficult drug to prescribe. So that needs to be a little more controlled, but we have it way too controlled and isolate it from the rest of medicine in a way that we don't do with any other drug. So, we have the tools to dramatically reduce the death toll for celebrities and for everybody else—we're just not using them.