Remnants of ancient virus may be fueling ALS in people
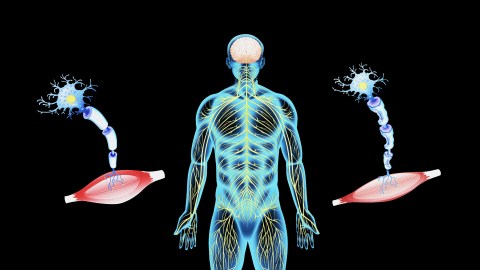
- Amyotrophic lateral sclerosis (ALS) is a fatal, neurodegenerative disease that attacks nerve cells in the brain and spinal cord; however, the cause is unknown.
- Scientists discovered that PEG10, a “domesticated viral gene” that is necessary for placenta development, builds up in ALS patients.
- They also found that PEG10 maintained some of its ancient viral functions and altered gene expression in a cell, including the expression of genes involved in nerve functions.
Amyotrophic lateral sclerosis (ALS) robs people of the ability to speak, move, eat, and breathe by attacking nerves. The disease is fatal and has no cure. Some people survive for three years, while others (most notably Stephen Hawking) survive for 50. CU Boulder researchers have identified a surprising new player in ALS — an ancient, virus-like protein best known for its essential role in enabling placental development.
Domestication of ancient viruses
Around 8% of the human genome is made up of bits of DNA left behind by viruses that infected our primate ancestors millions of years ago. Originally, these pieces of viral DNA encoded genes that helped a virus replicate and infect new cells. But over time this function was lost, and many of the ancient viral genes became junk. However, some of the genes have become domesticated, losing their ability to create new viruses but allowing their human hosts to evolve new adaptive functions.
PEG10, or Paternally Expressed Gene 10, is one such “domesticated viral gene.” Its viral origins are a mystery, but it is necessary for mammals to develop placentas. However, when PEG10 is overly abundant in the wrong places, it may also fuel disease, including certain cancers and neurological disorders. The recent study from the CU Boulder researchers, published in the journal eLife, has shown that PEG10 is present in high levels in the spinal cord tissue of ALS patients, where it likely interferes with the machinery enabling brain and nerve cells to communicate.
“Our work suggests that when this strange protein known as PEG10 is present at high levels in nerve tissue, it changes cell behavior in ways that contribute to ALS,” said senior author Alexandra Whiteley. “It is early days still, but the hope is this could potentially lead to an entirely new class of potential therapeutics to get at the root cause of this disease.”
Too much protein in the wrong places
Whiteley did not set out to study ALS or ancient viruses. Instead, her research team explores how cells eliminate extra protein, which can cause various neurodegenerative diseases, including Alzheimer’s and Parkinson’s. Her lab is one of a half-dozen in the world to study a class of genes called ubiquilins, which break down dysfunctional proteins and prevent them from accumulating in cells. In 2011, a study linked a mutation in the ubiquilin-2 gene (UBQLN2) to some cases of familial ALS, which makes up about 10% of ALS cases. The mutation causes UBQLN2 to function less efficiently, but how the faulty gene might contribute to ALS remained unclear.
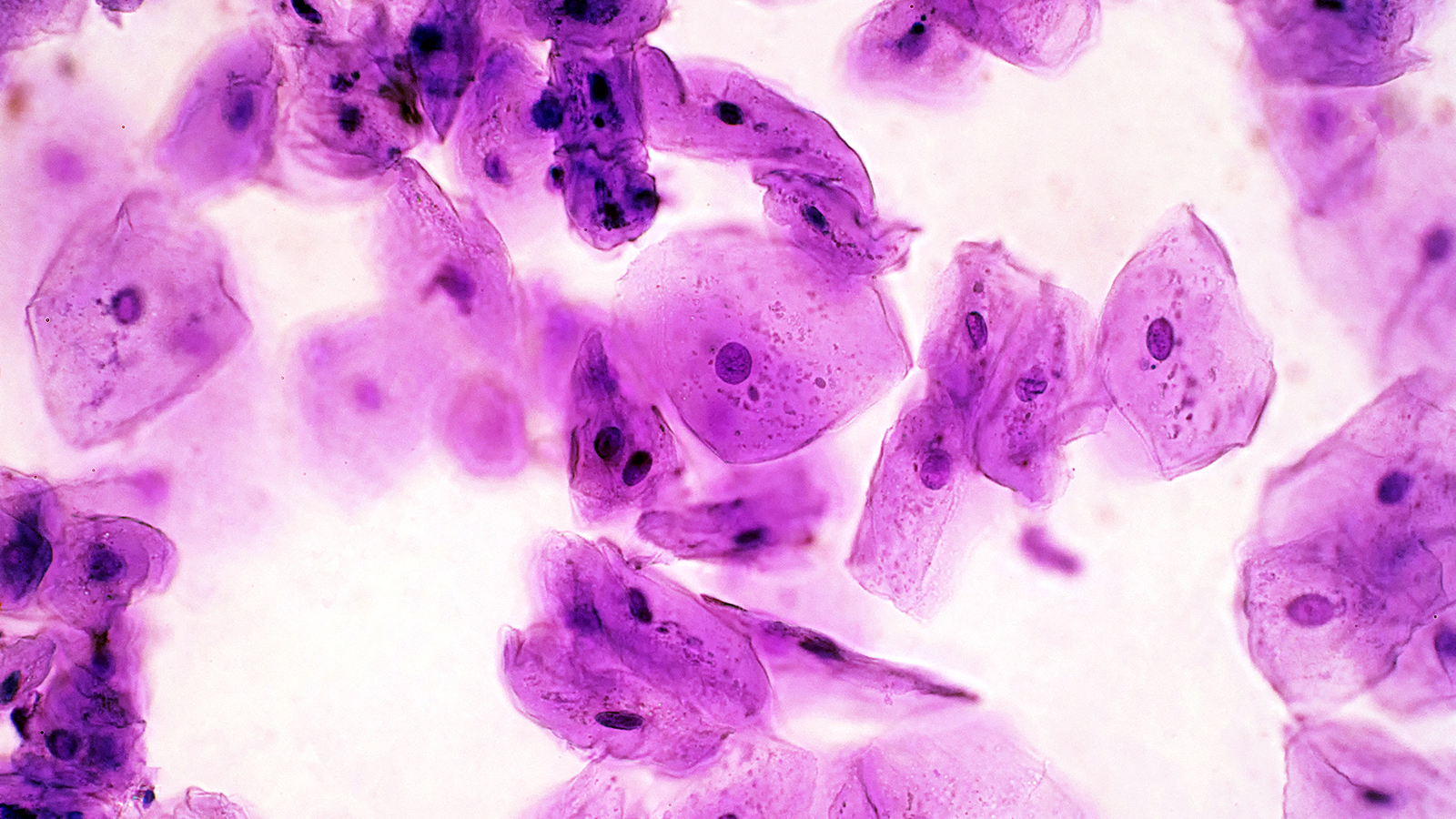
Whiteley suspected that defective UBQLN2 caused a build-up of protein that would otherwise be destroyed. So, Whiteley and colleagues at Harvard Medical School set out to determine which proteins pile up when the UBQLN2 is mutated. They collected the spinal tissue of 11 deceased ALS patients and analyzed the expression of more than 7,000 proteins. PEG10 was one of the most over-expressed proteins.
PEG10 still has some of its ancient viral functions
In a separate experiment, the team sought to determine how the overabundance of PEG10 was contributing to ALS. They found that the domesticated gene was not as domesticated as it seemed. As PEG10 built up in the cell, it altered its shape in a mechanism reminiscent of what viruses use to invade the nucleus of their host. Viruses use “nucleus-localized proteins” to influence gene expression to promote their own replication. The researchers found that the PEG10 fragment was sufficient to alter gene expression in a cell, including the expression of genes involved in axon remodeling, linking PEG10 dysregulation to neuronal dysfunction.
“The fact that PEG10 is likely contributing to this disease means we may have a new target for treating ALS,” she said. “For a terrible disease in which there are no effective therapeutics that lengthen lifespan more than a couple of months, that could be huge.”