A Woman Just Died From an Infection No U.S. Antibiotics Could Beat

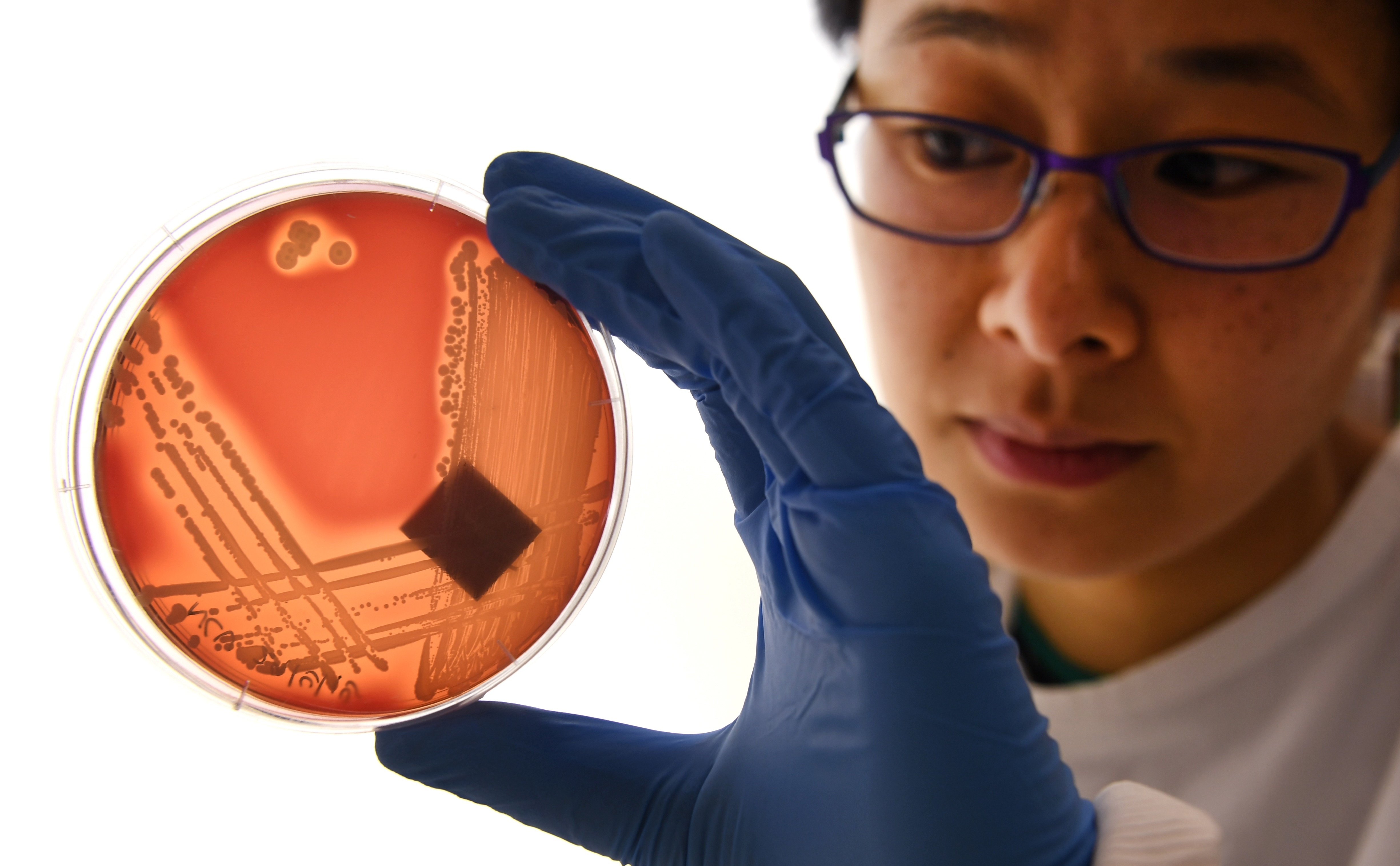
The woman from Washoe, Nevada was in her 70s and had an infection in her hip. She’d contracted it in a hospital in India after fracturing her leg. Doctors in Reno attempted to tame her infection, trying every antibiotic they had. 26 in all. None of them worked, not even colistin, their last line of defense. The woman died.
The CDC’s report on her case, issued January 13, is sending a chill through the medical world: They’ve been worried for years about the appearance of a superbug that beats all of our antibiotics. Is this what happened here? It turns out that maybe she could have been saved using an antibiotic called fosfomycin not approved in the U.S. for treating the kind of infection she had. Even so, her case has troubling implications.
Post-mortem testing of the woman’s bacteria revealed that something new is going on. Previous infections that have been resistant to treatment with colistin have had a single critical gene, MCR-1. This woman’s bacteria didn’t have this gene, so there’s some previously undiscovered mechanism at work.

Even prior to this, the protective firewall provided by colistin has been cracking. The drug was discovered in 1949 but went largely unused for a long time due to its harmful effect on the kidneys. It came to prominence as a last-line drug after bacteria strains showed signs of developing resistance to other key antibiotics — colistin had been so infrequently used meant that bacteria hadn’t yet had the chance to develop resistance to it.
But those days are apparently over. Colistin has become a popular, inexpensive additive to animal feed as both an antibiotic and also a way to quickly add muscle to animals. Agricultural demand for the drug reached 11,942 tons per year in 2015, and is expected to reach 16,500 tones by 2022. (73% of it is used in Asia, and 28.7% in Europe.) And the MCR-1 gene is now found in livestock and humans, suggesting that colistin’s days as a super-antibacterial are numbered.

One of the scariest aspects of the MCR-1 gene, by the way, is that it doesn’t live in a bacteria’s chromosome. Instead, it’s contained in a plasmid, a small, unattached bit of DNA. What’s worrisome about this is that, being independent, it can attach to any bacteria, thus making it resistant to colistin. The danger is that an MCR-1 plasmid, having been consumed in pork or chicken, attaches to some other bacteria it encounters in your gut. This is clearly already happening in patients carrying the MCR-1 gene. And it may a lethal recipe for the evolution of pan-resistant bacteria.
Fosfomycin, the antibiotic to which the woman’s bacteria showed some reaction post-mortem, is another old drug for which little resistance has yet been developed. It’s approved in the U.S. for treatment of urinary-tract infections, but not for intravenous use in fighting infections. Some wonder if and when the U.S. FDA will widen its availability for use.
As for the woman in Nevada, she was, thankfully, kept well-isolated from other patients and staff. Samples taken from the hospital have so far shown no sign of her bacteria anywhere, so a deadly outbreak seems to have been avoided. For now.