Vaccines. Time for Society to Say Enough is Enough

What does society do when one person’s behavior puts the greater community at risk? That’s a no-brainer, right? We make them stop. We pass laws, or impose economic rules, or find other way to discourage individual behaviors that threaten the greater common good. You don’t get to drive drunk. You don’t get to smoke in public places. You don’t even get to leave your house if you catch some particularly infectious disease.
Then what should we do about people who decline vaccination for themselves or their children, and put the greater public at risk by fueling the resurgence of nearly eradicated diseases? Isn’t this the same thing, one person’s perception of risk producing behaviors that put others at risk? Of course it is. Isn’t it time for society to say that in the greater public interest, we need to regulate the risk created by the fear of vaccines? Yes. It is.
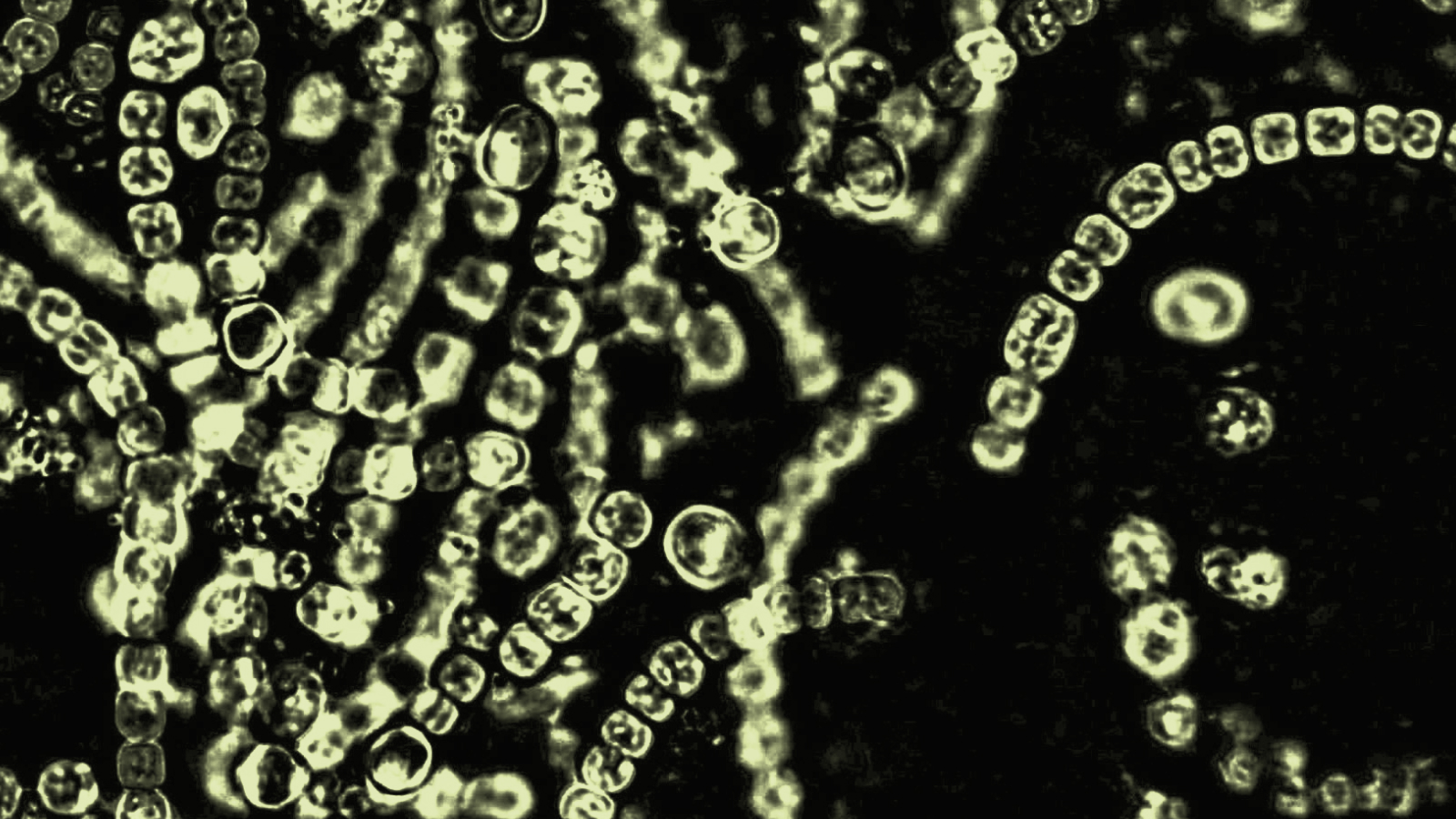
The evidence is overwhelming that declining vaccination rates are contributing to outbreaks of disease. Take just one example, measles. The WHO reports outbreaks in many countries where vaccination rates have gone down: As of June – France (12,699 cases in 2011, more than in all of 2010 already, including six deaths), Spain (2,261), Italy (1,500), Germany (1,193, one death), Switzerland (580), Romania, Belgium, Denmark, and Turkey. There have already been 550 measles cases in England and Wales this year compared with 33 all of last year.
The U.S. has seen 156 cases as of mid-June, compared to a total of 56 cases per year from 2001-2008. The CDC has an emergency health advisory out for measles, a disease officially declared eradicated in the United States in 2000.
Small numbers, you say? True, but consider their cost (beyond the suffering of the patients). Measles is ferociously infectious, and potentially deadly to the young or old or people with weakened immune systems, so it requires an intense response from the medical and public health communities. Consider just one small outbreak: When a woman from Switzerland who had not been vaccinated for measles visited Tucson and became symptomatic, she went in to a local hospital for medical attention and three months later at least 14 people, including seven kids, had gotten measles. Seven of the victims caught the disease while visiting health care facilities. Four people had to be hospitalized. The outbreak cost two local hospitals a total of nearly $800,000, and the state and local health departments tens of thousands more, to track down the cases, quarantine and treat the sick, and notify the thousands of people who might have been exposed.
Fueling the spread? None of the victims had been vaccinated, and, remarkably, 25% of the workers in the health care facilities where the patients were treated had no immunity to measles (either they had not been vaccinated or the antibodies from an earlier vaccination could no longer be detected in their blood stream.) One health care worker got the disease, and gave it to two other people.
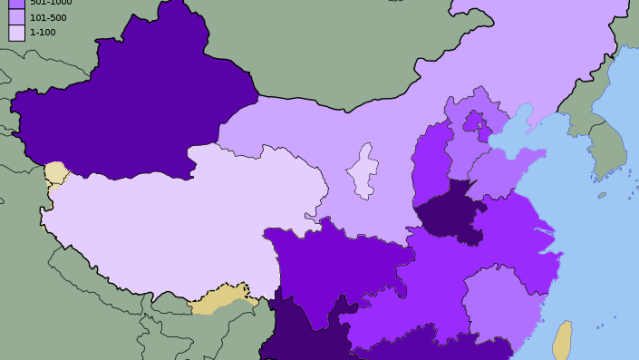
That’s just one example of the growing threat to public health caused by people worried that vaccines will cause autism and other harms, despite overwhelming evidence to the contrary. In many places, particularly in affluent, liberal, educated communities (Boulder, San Diego), unvaccinated people are catching diseases that vaccines can prevent, like measles, whooping cough, and meningitis. In 2010 as California suffered its worst whooping cough outbreak in more than 60 years (more than 9,000 cases, 10 infant deaths), Marin County, one of the richest and most educated areas in California, had one of the lowest rates of vaccination statewide and the second highest rate of whopping cough. A 2008 study in Michigan found that areas with “exemption clusters” of parents who didn’t vaccinate their kids were three times more likely to have outbreaks of whooping cough than where vaccination rates matched the state average.
And this is a risk to far more people than just those who have opted out of vaccination. People are getting sick who have been vaccinated but the vaccine either doesn’t work or has weakened. (Of the 156 measles victims in the U.S. as of June, nearly one in five of them had been vaccinated but the vaccine didn’t work, or had weakened.) Infants too young to be vaccinated are getting sick, and some of them are dying, when exposed to diseases in communities where ‘herd immunity’ has fallen too low to keep the spread of the disease in check. Unvaccinated people are getting sick and visiting doctor’s offices or hospitals seeking treatment, raising the risk to anyone sharing those facilities, costing the health care system millions of dollars in avoidable expense, and costing local and state government (that’s taxpayer money, yours and mine) millions more as they try to chase down each outbreak and bring it under control, to protect the public’s health. Your health, and mine. (A recent economic analysis found that “…vaccination of each U.S. birth cohort with the current childhood immunization schedule prevents approximately 42,000 deaths and 20 million cases of disease, with net savings of nearly $14 billion in direct costs and $69 billion in total societal costs.
It is time to act in the face of this threat. This is not to deny the feelings of those who fear vaccines, or denigrate those fears as irrational, as many in the health care and vaccine communities too readily do. In fact, this is to recognize and respect the honest and powerfully deep roots of those fears, and the fact that no amount of communication or dialogue or reasoning can make people really worried about vaccines, stop worrying. Risk perception is ultimately subjective, a combination of the facts and how those facts feel. Sometimes our fears just don’t match the facts, and the gap between our feelings and the evidence, what I call “The Perception Gap”, produces real risks all by itself, risks which need to be managed the same way society tries to manage myriad other threats to public health from which we can’t protect ourselves as individuals.
There are many potential solutions, each fraught with pros and cons and details that require study and careful thought and open democratic discussion.
— Perhaps it should be harder to opt out of vaccination. (Twenty-one states allow parents to decline vaccination of their children simply for “philosophical” reasons. 48 allow a religious exemption but few demand documentation from parents to support claims that their faith precludes vaccination.)
— Perhaps there should be higher health care/insurance costs for unvaccinated people.
— Or we could do it in a positive way, with reduced health care/insurance costs for people who do get vaccinated, ‘healthy behavior’ discounts paid for by what society saves by avoiding the spread of disease.
— There could be restrictions on the community/social facilities unvaccinated people can use, or limits on the social activities in which they can participate, like lengthy school trips for kids, etc.
— Here’s an idea; vaccination, including boosters, should be required of anyone who wants to work in health care.
This is not about creating more government to intrude further into our lives. There is already too much of that. This is about calling on government to do what it’s there for in the first place, to protect us from the actions of others when we can’t protect ourselves as individuals. We do this in countless ways already. It is appropriate, and urgent, that we act to protect ourselves from those whose choices about vaccines are putting the rest of us at risk, and do the same thing society always does whenever one person’s behavior endangers the greater community. We make them stop.