HIV Vaccine: Do Babies’ Immune Systems Hold the Key?

HIV/AIDS research has come a long way. Though first introduced to human hosts in West Africa at the turn of the previous century, the first case of HIV/AIDS wasn’t recorded until 1959. Yet, it didn’t enter into the collective psyche until 1981, when gay men were mysteriously dying from a disease which gave pneumonia-like symptoms, before compromising their immune systems and taking the their lives.
By 1994, AIDS was the leading cause of death among those ages 25-44. Luckily a year later, highly active antiretroviral therapy (HAART) were discovered. They made it to market by 1997. This is a mix of medications which stops the virus from replicating. In 2012, a prescription medication called Truvada was made available, though it still isn’t being marketed. Also known as pre-exposure prophylaxis (PrEP), the drug can bring one’s viral load down so low it is undetectable. It can also prevent the transmission of HIV, if taken regularly.

Truvada also known as PrEP or antiretroviral drugs (ART).
Though we can prevent HIV from turning into full-blown AIDS, we cannot cure it. The virus hides in areas of the body known as reservoirs, biding its time, and looking for an opportunity to resurface. What’s more, even though patients on these drugs can live normal, healthy lives, a recent study found that HIV patients on such drugs experience severe age-related diseases, such as heart disease and cancer, five years earlier than their peers. A few novel approaches are out there, including a strategy known as “kick and kill,” which pushes the virus out of its hiding spot and eliminates it. Still, we are still far from a cure. This is truly one of the most complex diseases medical science has ever faced.
Besides a cure, the other approach would be a vaccine. But this too has proven elusive because adult immune systems respond much too slowly to the virus. By the time protection has been built up, the virus has already countered it. Now a team of researchers from the Fred Hutchinson Cancer Research Center in Seattle, believe they have a way of devising one. Studying the immune systems of infected infants, researchers believe that if they can mimic a baby’s immune response, they may be able to create the world’s first HIV vaccine.

Model of the HIV virus.
Published in the journal Cell, researchers studied babies born to infected mothers in Kenya, years before antiretroviral drugs were available. They found that broadly neutralizing HIV antibodies can be detected in infants within a year after becoming infected. Not only do the antibodies need to be produced quickly, there has to be the right mix of them to identify and eliminate the virus. The immune system must also be able to quickly adapt to the virus. Thus antibodies, which have passed through the process of “somatic hypermutation,” are required. This is the ability to block and bind to pathogens, an essential part of the immune response.
It can take years or even decades for an adult immune system to mount a response capable of protecting the body against HIV. Due to this, a vaccine has been impossible to create. This study builds upon a previous one which discovered, unexpectedly, that broadly neutralizing antibodies were in fact created early on in life. Not only can the infant immune system produce such antibodies in less than a year, a vaccine could be culled from this with less finagling than previously thought. Though this is great progress, there is still a long way to go. A vaccine needs to be able to trigger an immune response within months of infection, not a year or more.

HIV virus (in green) attacking immune cells.
Researchers used blood samples from infected infants, who were part of a breast feeding study within the Kenya Research Program. The Seattle team examined antibodies and the antibody response within the infants’ blood. One baby in particular was HIV-negative birth. It was found to be infected by four months of age, perhaps due to breastfeeding.
Dr. Julie Overbaugh was the senior author in this study. She leads a lab within the research center which investigates HIV transmission and development. Dr. Overbaugh said that adults have immune responses driven by one specific kind of antibody. However polyclonal responses, or those with several different kinds of antibodies, are harder for the virus to avoid. It is also much more difficult to protect itself from. So not only was a baby’s immune system faster, it approached HIV in a multi-faceted way.

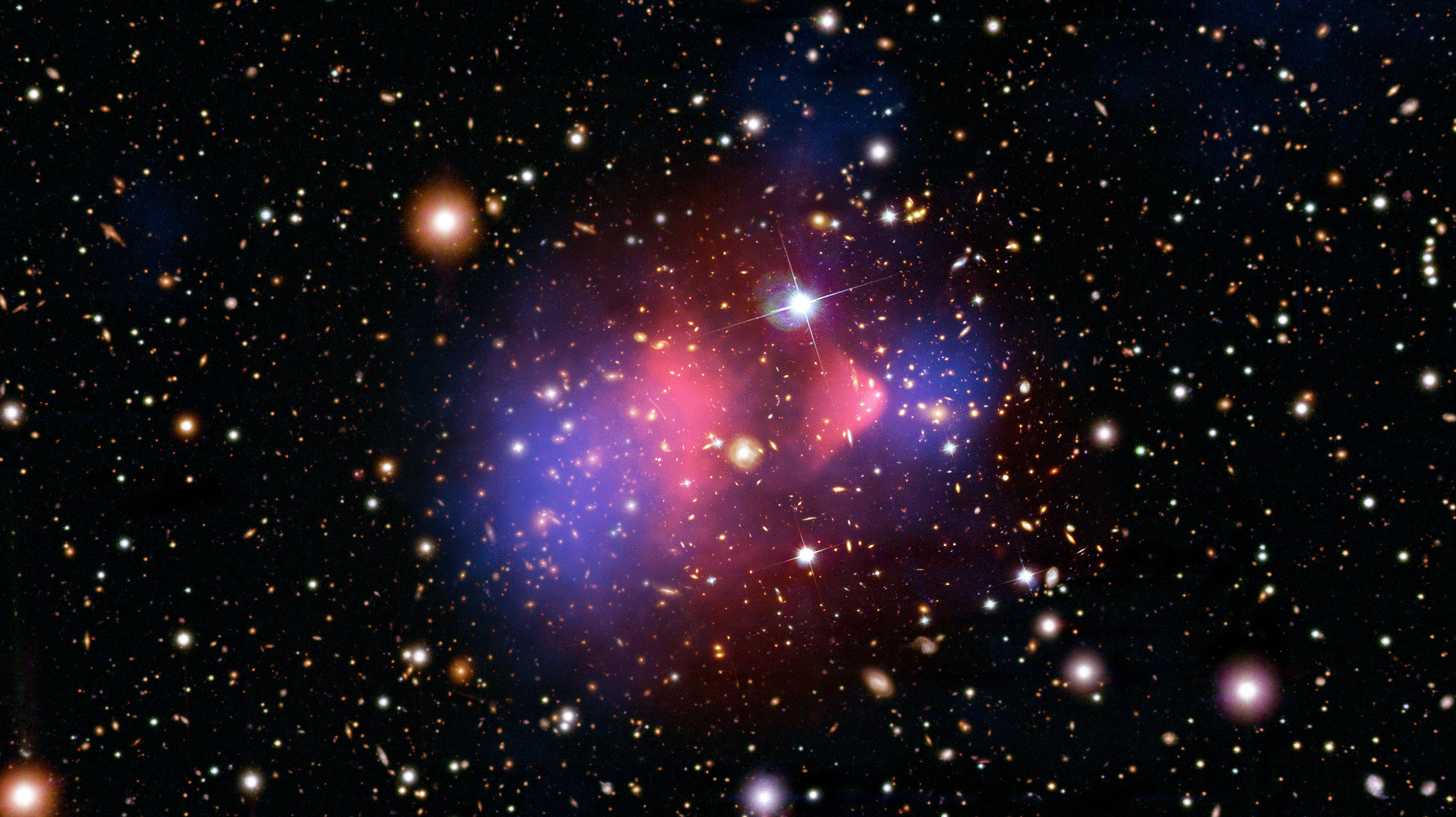
HIV infection rates globally.
The team also found that infant antibodies target different sites on HIV than adult ones do. This might suggest a unique kind of protection occurring in early life. Dr. Overbaugh and her team say that these quickly-produced, broadly neutralizing antibodies could lead to a vaccine. Even so, this breakthrough leaves more questions than answers.
For instance, why exactly was the immune response different in babies? And why are these unique features lost later on in life? One theory is that the infants were already exposed to the virus through the mother’s immune system, giving them the upper hand after birth. Otherwise, it may turn out that babies have an immune system capable of providing extra protection in early life. More research will be needed to confirm these results, and to further understand what forces are at work. But researchers are optimistic that a vaccine may someday soon be within reach.
To learn more about a cure for HIV click here: