“Love hormone” oxytocin literally heals a broken heart

The “love hormone” oxytocin creates social bonds and generates the pleasurable feelings associated with art, exercise, and sex. Now, researchers show that the love hormone has an unsuspected function: It can help mend a broken heart. According to their study, oxytocin stimulates stem cells to develop into cardiomyocytes — the muscle cells that generate heart contractions and which are damaged during a heart attack.
When the heart doesn’t get enough oxygen, cardiomyocytes die. Fortunately, these cells can be regenerated by a subset of stem-like cells called epicardium-derived progenitor cells (EpiPCs). Unfortunately, humans are terrible at producing EpiPCs. Instead, an injured heart typically resorts to replacing the dead cells with scar tissue. This short-term solution often leads to heart failure if left untreated. Therefore, Aitor Aguirre, an assistant professor at Michigan State University, wanted to discover a way to induce cardiomyocyte regeneration and subsequently restore cardiac function.
The healing power of the brain
To heal a damaged heart, Aguirre looked to the brain. Neural structures, such as the hypothalamus and pituitary, regulate normal cardiovascular functions like heart rate and blood pressure by releasing various hormones. Additionally, studies in zebrafish have found that several hormones affect cardiac regeneration. For example, estrogen accelerates regeneration, and cortisol reduces regeneration. Furthermore, a recent study in young African clawed frogs, which are capable of scar-free healing and regeneration, indicates that damage to the hypothalamus inhibits regenerative processes in vertebrates. Because of these studies, Aguirre hypothesized that the brain releases hormones after cardiac injury to facilitate heart regeneration. If he could identify these hormones, they could be used to accelerate regeneration.
Aguirre and his team identified 15 candidates, including growth hormone (which is undergoing clinical studies to determine muscle regeneration in severely burned patients), prolactin (which regulates liver regeneration in mice), and oxytocin (which is necessary for muscle maintenance and regeneration). The scientists added the hormones to human EpiPCs to determine if they might affect heart regeneration. They found that oxytocin had the most potent effect: It increased the EpiPCs’ ability to proliferate three-fold compared to untreated cells, a much stronger impact than other molecules previously shown to stimulate EpiPC production in mice.
The love hormone is necessary for heart regeneration in vivo
The researchers wanted to determine if oxytocin was necessary for heart regeneration in a living organism. To do this, Aguirre and his team turned their attention to the masters of organ regeneration: the zebrafish. Zebrafish have an extraordinary capacity for regenerating organs, including the brain, retina, internal organs, bone, and skin. They don’t suffer heart attacks, but many predators are happy to nibble on zebrafish organs, including the heart. Similar to humans, zebrafish rely on EpiPCs.
The researchers opened the fish’s chest cavity to induce damage, revealing its beating heart. Then, they gently placed a liquid nitrogen-cooled metal probe on the tip of the heart for about 45 seconds. Finally, Aguirre and his team sewed the cavity closed and returned the fish to their aquarium. Within three days after cryo-injury, oxytocin RNA expression in the brain increased 18-fold and lasted for at least seven days, suggesting that a burst of oxytocin is released from the brain into the bloodstream after cardiac injury over a sustained period.
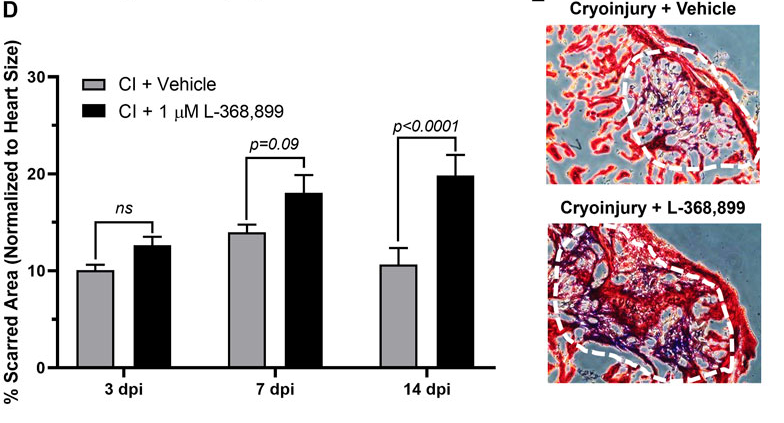
To determine if that burst of love hormone is necessary for regenerating heart tissue, the researchers injected some of the cyro-injured zebrafish with an oxytocin inhibitor. They found that these zebrafish healed over time; however, their hearts contained much more scar tissue than uninhibited fish.
“These results show that it is likely that the stimulation by oxytocin of EpiPC production is evolutionary [sic] conserved in humans to a significant extent. Oxytocin is widely used in the clinic for other reasons, so repurposing for patients after heart damage is not a long stretch of the imagination. Even if heart regeneration is only partial, the benefits for patients could be enormous,” Aguirre said in a statement.
“Next, we need to look at oxytocin in humans after cardiac injury. Oxytocin itself is short-lived in the circulation, so its effects in humans might be hindered by that. Drugs specifically designed with a longer half-life or more potency might be useful in this setting. Overall, pre-clinical trials in animals and clinical trials in humans are necessary to move forward.”