The End of Free Will?

What’s the Big Idea?
The field of neuroscience evolved so rapidly in the past twenty years that it will pose unprecedented challenges to the legal system in the decades to come, changing the way we understand crime and punishment, says neuro-pioneer Joy Hirsch, director of the Functional Magnetic Resonance Imaging Center at Columbia.
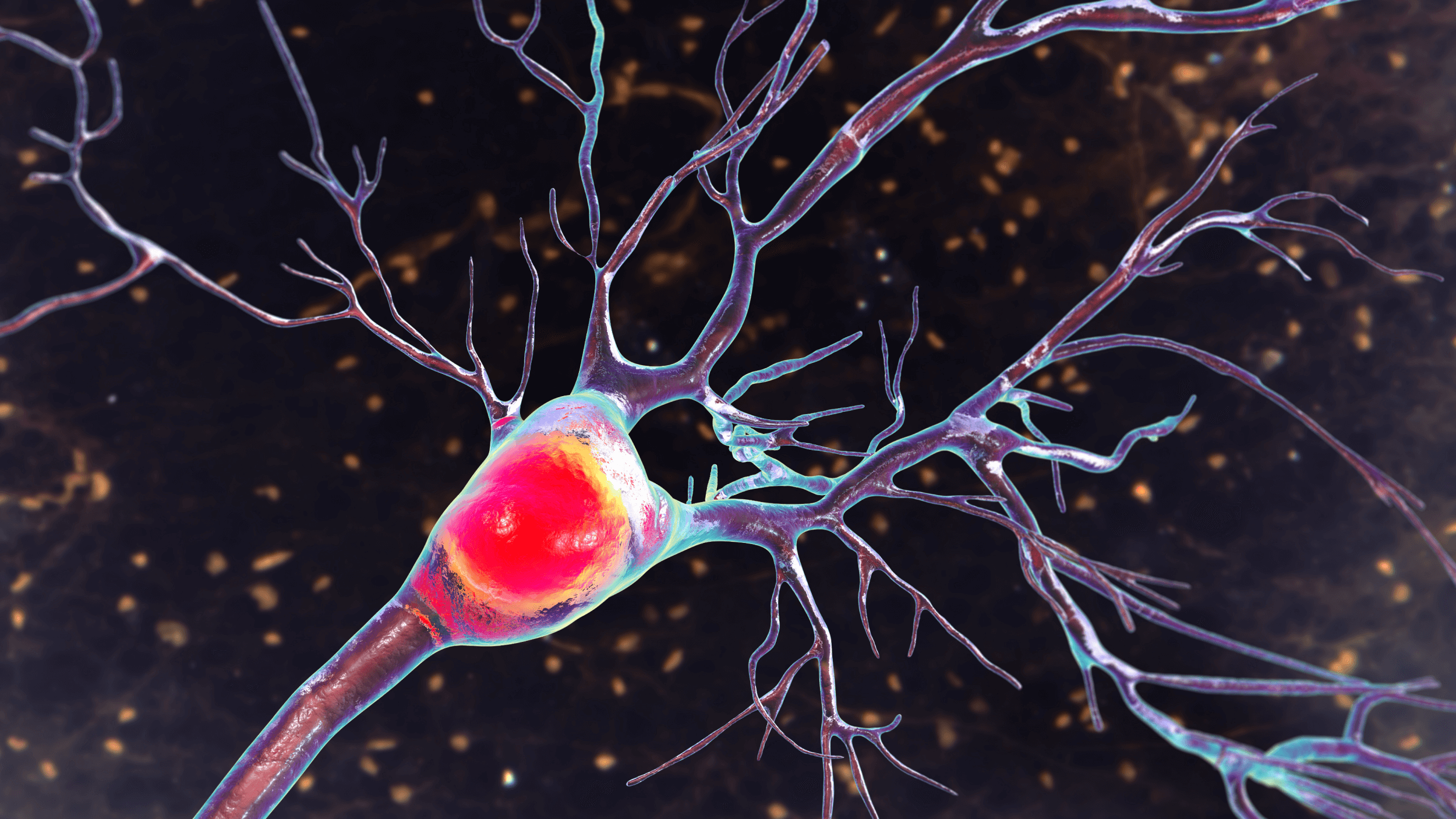
Functional imaging, for instance, has given scientists the ability to identify which specific areas of the brain are active during specific tasks. It’s a development that Hirsch compares to manna from heaven.
“I was at Kettering in 1991, when the blood oxygen level dependent signal – the primary signal of functional imaging – was discovered,” she says. “I had a feeling that this was going to change the course of neuroscience, because if that signal was real then it meant that we would actually be able to observe, physiologically, the function of the brain that we had made inferences about from more or less the black box system of study.”
By 2005, a technique utilizing this knowledge had been adopted by the AMA, resulting in widespread use in research and community hospitals across the country. Over the course of about five years, the way surgeons plan and execute operations was entirely revised.
Now, imaging technology creates a map of the patient’s brain, allowing his or her surgeon to pinpoint the areas most vital to the performance of tasks memory storage and sight in that individual patient. Before operating, a surgeon knows exactly where to cut and what to avoid.
“It’s [one] example of [an application] that has gone all the way from the bench stage, the place where the science actually happened, to the bed stage, where patients actually benefit from the new procedure,” says Hirsch. “We’ve begun to tap in to the dynamics of the language of the brain as opposed to just understanding specific areas.”
But the specificity and intimacy of such knowledge is alarming. After all, we’re talking about unlocking access to a person’s unique set of mental processes and interactions. Should brain images be admitted as evidence in court? Could they be used to defend someone with an abnormality, such as a brain tumor, which might impair judgment?
What’s the Significance?
Those in the legal professors are very interested in developments in neuroscience, says Hirsch, and rightfully so. Last year, she was asked to give a keynote address on “Neuroscience and Law” at the education conference of the Second Circuit Court Judge in New York. There were two questions on everyone’s mind. Both were concerned with free will and the extent to which we can ever actually know another person’s experience.
If someone has a brain tumor in the frontal lobe (which we know is associated with areas involving judgment), is that person as responsible for a violent crime as someone with a brain that is not known to have a specific anomaly?
Hirsch responds: There is no black and white answer here. There are arguments that go back and forth – but I’m very comforted by the fact that the legal system is taking these issues, these very important issues, in a thoughtful, contemplative manner… The law will emerge, but no one can predict exactly how or how precedent will be established.
Can one read the brain and make inferences about what is actually being experienced by that individual?
Hirsch responds: This question is a little bit less philosophical and more operational. It applies to the documentation of personal injury as it relates to conditions like chronic pain. Pain is one of these sensory perceptions that falls in the category of the hard problem, that is, how do I know that your sensation is pain just because you tell me you’re in pain, when I don’t see an injury that makes me think you’re in pain.
How do I know that your complaint of chronic pain is real? Functional imaging has been shown to be very effective in documenting sensory responses, neurological responses, associated with mechanisms that we know are related to pain. The general consensus is moving toward the possibility that functional imaging might be legitimately entered as evidence into a course of law documenting personal injury type of experiences.
Whenever you experiment, there are risks, she says, but in this case, the greater good – the potential to alleviate unnecessary suffering – outweighs the possibility that moving forward with brain research might be harmful. In the near future, enhancement of the brain with mechanical and electric assists (prostheses that enhance or delete incoming information) could open up new therapeutic possibilities for those with anxiety, depression, and autism. Hirsch and her team recently published a paper in the scientific journal Radiology proposing a diagnostic framework for autism using MRIs of language systems in the brain to differentiate children with autism from those without it.
Tell us: Do you agree with Hirsch that neuroscientists should be able to move forward with research into brain enhancements? What is the most important ethical issue that we will face in the next decade, due to developments in neuroscience?