Harvard Professor David Scadden discusses the wonder of self-replenishing stems cells, and reveals scientific findings that might enable any stem cell to be reprogrammed as an embryonic stem cell.
Question: What are stem cells?
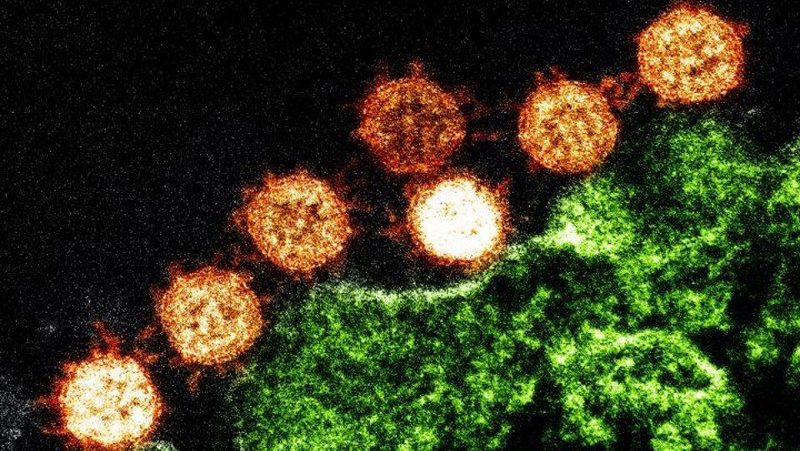
David Scadden: Well, stem cell is a very unique concept; actually it’s a wonderful very creative notion of a single cell that has the capacity when it divides to give a reproduction of itself as well as one cell going off to become all the other cells that can make up of tissue or organ of the whole body. So, it has this really unusual characteristic of these two outcomes from a single division.
Most cell types, they’re either moving their way progressively towards something that is more defined, more specialized, more restricted in what it can do. And they also have the capacity to; they don’t have the capacity to sexually renew. And so they’re basically moving down the road toward self destruction. They end up generally having fairly short half life, and some cells live a long time. But then they’re not actually dividing things like a heart cell or brain cell. Those are generally fairly stable; they don’t divide very much if ever. And they can live for a while, but a cell that has a capacity to generate new cells and yet restore itself. So it’s a self-replenishing resource. It’s a very unusual entity. It’s really quite a wonderful concept actually.
Question: What kinds of stem cells are there?
David Scadden: There are different kinds of stem cells. What has generated the most controversy is this so called embryonic stem cell that comes from a very early stage in development; it is after the first week to ten days following fertilization in human. Those cells have unique capability to become virtually any cell type, so they’re called Pluripotent. Most cells after that time are much more restricted on what they can become. But stem cells of this more restricted nature stay with us throughout life. So we all have stem cells. These are cells that are capable of forming for example all the cells of the blood. So a blood stem cell is a very important part of active therapy today. We have those in the skin, we have those in the skeleton, we have those in the intestine, we have many of those different adult stem cell types, but they are limited to what they can become. They can’t have the ability for let’s say, a blood stem cell to become a nerve cell where as these other pluripotent cells can. Now though that divide between the pluripotent stem cell or embryonic stem cell and the adult stem cell was something that was thought to be unbridgeable gap, but over the last three years, there’s been a revolution in that we now have the ability to take essentially any mature cell type and convert it back into one of these pluripotent cells. So there’s been a tremendous shift in thinking and capability in the stem cell arena. Because now it seems any cell can be made to become a stem cell. It’s a really phenomenal concept.
Topic: Stem cells and the healthcare industry.
David Scadden: This idea that you could regenerate tissue is one that could really potentially reverse some of the calculus of how any new medical intervention means, such an incremental additive cost. We’re hoping that if we really can accomplish even part of the promise of stem cells that we’ll be able to put back in place tissue that might otherwise have been damaged. If that tissue is capable of sustaining function, what that could do would be to reverse some of the disability. It could reverse some of the dependence on chronic care. If we could improve the heart function of individuals who have terrible heart failure. Well those individuals are entirely are bed-ridden and are highly dependent on health care providers and their family and on medicines. If we can provide some of that function. If we can restore some degree of independence, the impact of individual life would be enormous. If we think about multiplying that in terms of its impact on those care providers, those health care needs, the societal implications could be really, actually quite dramatic.
And so we’re hoping that the investment in this area is one that will in many ways generate a return that may have a potential of lowering our health care cost. If this is something that really offers a chance to reduce disability, we have to explore that. It’s really something that our health care system so needs now as a way to try to reduce some of the cost. So, I’m actually quite excited that this field, if it can be moved ahead in rapid pace, might actually come to play at a really a critical moment in our health care delivery system. We’re clearly getting to the point where we almost have an unsustainable level of cost. Maybe if we have something that intervenes, creates greater ability that people can gage, but gage in more healthy way, less disability. Well that has a great deal of impact on our national productivity, health care cost would be enormously invaluable resource. So, maybe a bit grandiose but I’d like to think that this science is one that could really have societal implications that would be very positive on many fronts.
Recorded on: July 06, 2009