Is Your Diet Fighting Depression – or Intensifying It?

Scientists have recently become aware there’s a connection between our gut and our brain. But just how deep does this connection go? Could we, say, treat depression just by adopting a Mediterranean diet? A new study suggests, yes.
Doctors have been prescribing diets to their patients as a preventative measure against heart disease, cancer, diabetes, and now depression joins that list. “We now have real evidence to back up what’s good common sense: that eating well doesn’t just benefit your body, but it also benefits your brain,” says Columbia professor Drew Ramsey, who wrote, Eat Complete.
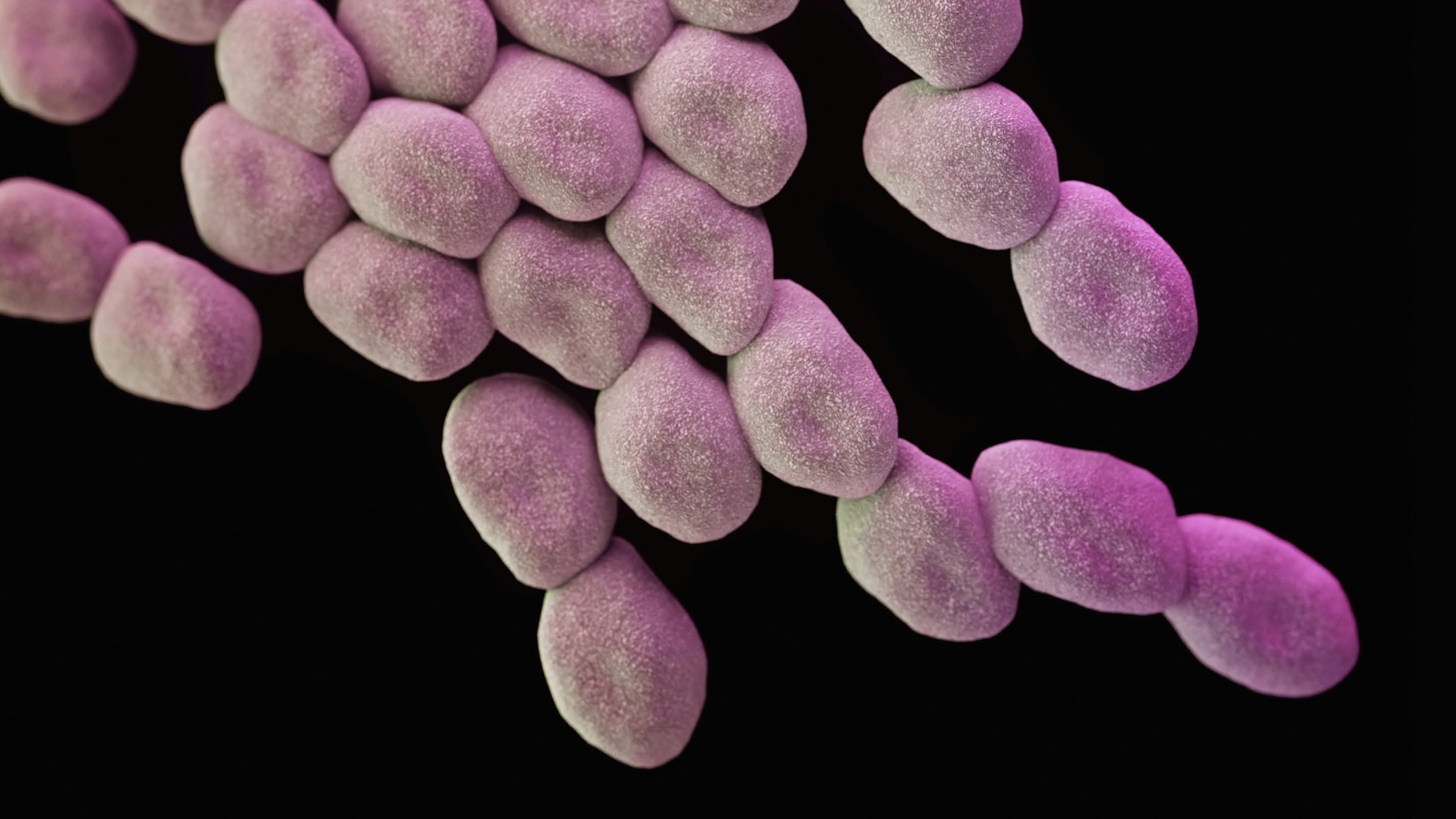
Ramsey represents a growing group of mental health experts who practice nutritional psychiatry. The idea of a gut-brain connection is one that has been gaining ground in scientific studies and some have started putting these ideas into practice. There’s evidence to suggest certain foods influence the bacteria in our gut, which in turn influence mental health.
It’s also important to note about 95 percent of your body’s serotonin is made in your gastrointestinal tract. Scientists are just beginning to discover this secret life of microbes and how much they influence other aspects of our overall health and wellbeing. But we can influence our microbiome with what we eat.
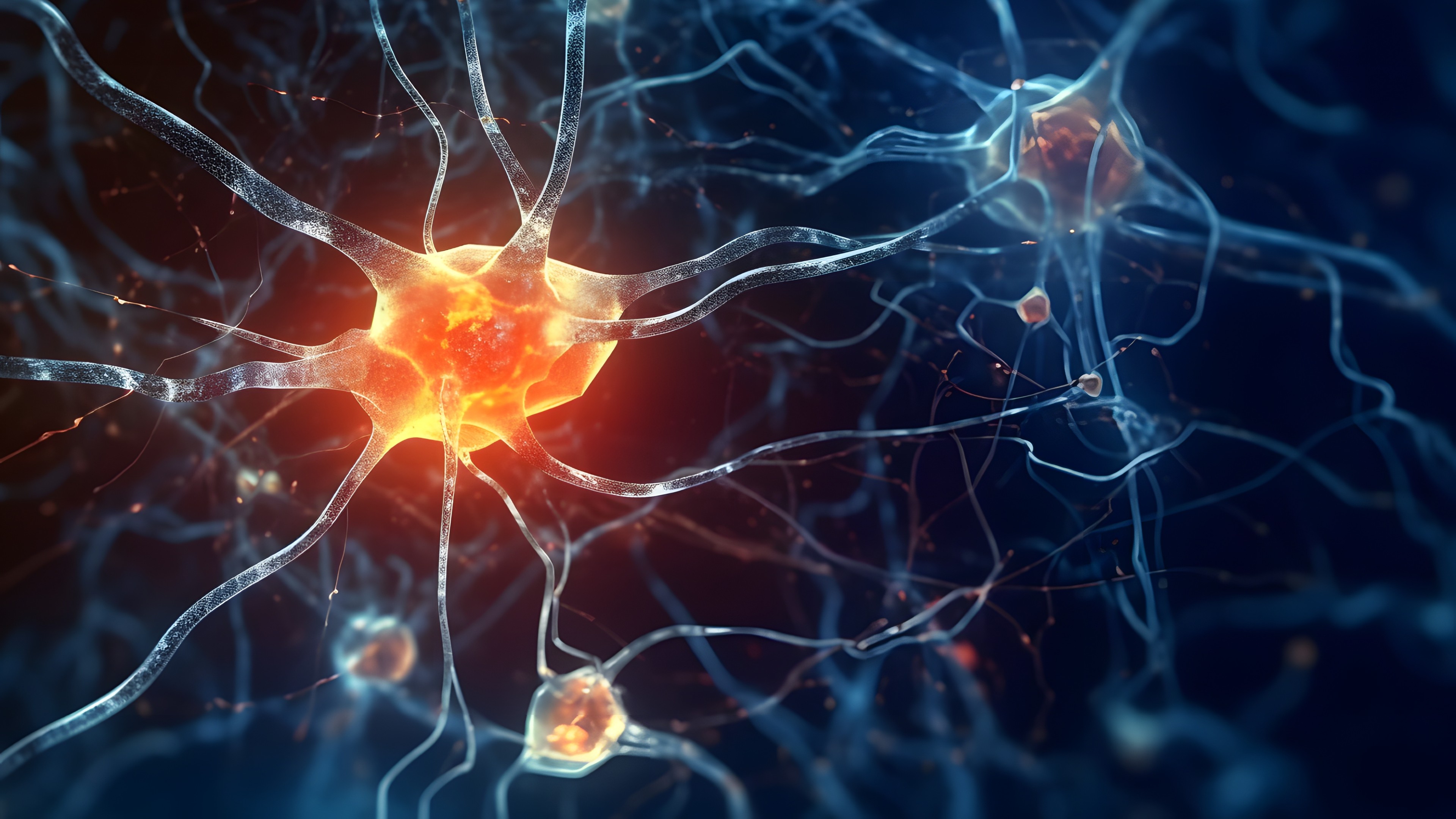
The brain is also directly affected by diet. “Tryptophan is the amino acid that we use to make serotonin and dopamine,” Ramsey told us when he came to Big Think. “These are very, very important mood-regulating and learning-regulating neurotransmitters, or chemicals in the brain. And so the idea is to give people a core set of foods. You know, again, with every bite you’re getting all the nutrients that your brain needs.”
Researchers from Australia’s Deakin University led a controlled clinical trial which gives promising results towards suggesting “dietary improvement guided by a clinical dietician may provide an efficacious treatment strategy for the management of this highly prevalent mental disorder.” The researchers recruited several hundred patients with moderate to severe depression, 67 of whom participated in a 12-week parallel group trial. All participants had poor dietary quality when they entered the trail, meaning they ate empty carbs and nutrient-sparse foods, like pizza, pasta and baked goods – what Ramsey terms the “beige diet” or the “12-year-old boy diet”.
Ramsey explains the trial result that is exciting for the future of mental health treatment:
“The augmentation effect was quite robust for an adjunctive treatment. In the treatment group, about 32% of patients achieved remission, compared with 8% in the control group. In terms of risk-benefit profiles, a dietary intervention is emerging as a very safe and effective way for us to engage our patients.”
The promising meal plan has been coined the Modi-Medi Diet – or modified mediterranean diet –and consists of legumes, leafy greens, colorful vegetables, a variety of quality seafood, quality lean red meat, fruits, olive oil, and nuts. Ramsey emphasizes that the quality of food, in particular of meat and seafood, is important – which is often an area of concern for people trying to make a positive diet change: organic food is expensive. During the trial, the Australian researchers actually found that eating the right foods for optimal brain health is cheaper. “The average Australian spends $138 a week on food. Those who were taking part in the study spent just $112,” says Ramsey. What is it about these foods that boost brain function and mental health? They contain nutrients the brain needs, specifically omega-3 fats, zinc, magnesium, iron, and vitamin B12, which are “highly correlated with a lower risk for depression and dementia.”
It’s important to note, the field of nutritional psychiatry is still new, so you should not use this diet as a substitute for consulting a therapist if you feel depressed.