Single dose of psilocybin reduces depression in phase 2 trial

Can psilocybin serve as a uniquely powerful and long-lasting treatment for depression? Since the renaissance of psychedelic research emerged in the 2000s, a growing body of studies suggests that psilocybin can reduce symptoms of conditions like major depressive disorder, anxiety, and end-of-life distress.
The most intriguing findings center on dosage: Some studies suggest that a single dose of psilocybin can yield therapeutic benefits that last long after the drug’s hallucinogenic effects wear off, possibly even months after ingesting one dose.
A study recently published in JAMA sheds new light on the therapeutic potential of psilocybin for depression. The randomized, double-blind phase 2 trial, conducted between 2019 and 2022, investigated the effects of a single dose of synthetic psilocybin on people with major depressive disorder.
The researchers found that “a 25-mg dose of psilocybin administered with psychological support was associated with a rapid and sustained antidepressant effect, measured as change in depressive symptom scores, compared with active placebo.”
Here are some of the key takeaways:
- The recent study featured a sample size of 104 people and a longer follow-up period than many previous studies on psilocybin and depression.
- The participants who received psilocybin showed significantly reduced depressive symptoms compared to those who received a placebo, though they also experienced more adverse events.
- The improvements in depression were sustained over a six-week follow-up period.
“These findings add to evidence that psilocybin—when administered with psychological support—may hold promise as a novel intervention for [major depressive disorder],” the researchers noted.
The results are promising, though they come with a couple of caveats.
A closer look at psilocybin and depression
For the study, the researchers recruited a total of 104 adult participants with moderate to severe major depressive disorder. After participants were given time, if needed, to stop psychotherapy and taper off any antidepressant medications they were taking, the researchers randomly sorted them into two groups.
One group of 51 people were assigned to get a single dose of psilocybin. The other group of 54 participants were given a placebo: niacin, a B vitamin that causes your face to “flush.” (The idea is that this reaction might make it harder for people to tell whether they got the drug or the placebo.) At the start of the study, neither the researchers nor the participants were told who received the psilocybin. Also, participants were given multiple sessions of psychological support, including during the psilocybin (or niacin) experience.
The main goal of the study was not to see whether depression decreased while people were experiencing the effects of psilocybin but rather to track changes in depressive symptoms in both groups at various timeframes over a six-week follow-up period. To do that, the researchers measured participants’ scores on the Montgomery-Asberg Depression Rating Scale (MADRS), which assesses the severity of depressive episodes. The researchers also had participants complete the Sheehan Disability Scale (SDS), which measures how symptoms impair functioning in daily life.
Participants completed both scales before taking either the psilocybin or the placebo, referred to as their baseline score, and also at follow-up periods: 2, 8, 15, 29, and 43 days after dosing.
The results revealed a statistically significant difference between the two groups in terms of reduced depressive symptoms over the six-week period. The group that got psilocybin saw their MADRS scores decline by an average of 19.1 points, vs. 6.8 points in the placebo group.
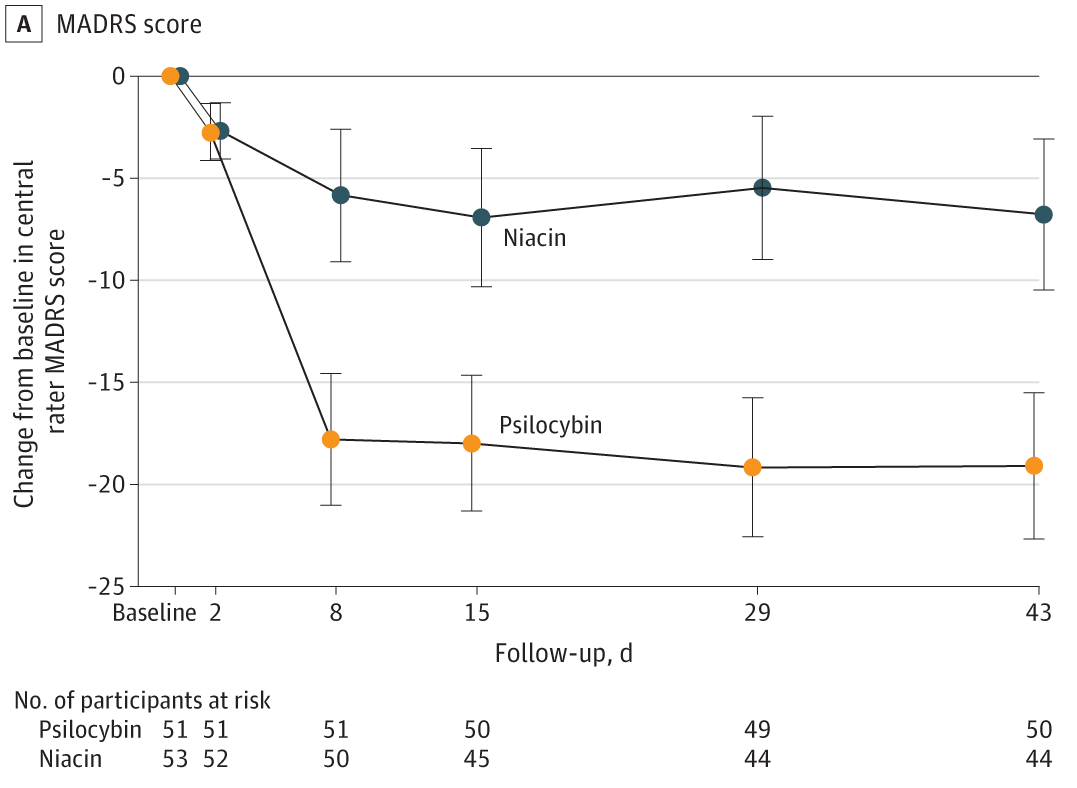
By day 43, 58% of participants in the psilocybin group demonstrated a sustained response (defined as a 50% reduction from their baseline score), compared to 20% of the placebo group.
Although a sustained response is a good sign that an antidepressant is effective, it’s not the same as sustained remission, where depressive symptoms drop into the “normal” range. (While a greater share of the psilocybin group did go into remission compared to placebo, the difference wasn’t statistically significant.)
When it came to safety and tolerability, the researchers wrote, “Psilocybin was generally well-tolerated, with most AEs [adverse events] being of mild or moderate severity and generally limited to the acute dosing period.” However: “psilocybin treatment was associated with a higher rate of overall AEs and a higher rate of severe AEs compared with niacin, with these severe AEs being known effects of psilocybin.”
Caveats and cautious optimism
It’s worth noting that not all participants stuck with the follow-ups. The placebo group had a higher dropout rate, with 44 of the initial 53 participants ultimately making it to the 43-day check-up. Meanwhile, all but one participant in the psilocybin group completed the study (one withdrew from the study due to a death in their family).
What explains the difference in dropout rates? It’s hard to say for sure, but one possibility is that people in the placebo group became less motivated to participate in the study because they knew they received niacin instead of psilocybin. This underscores what’s arguably the biggest problem with psychedelic research: complications with blinding.
To validate the therapeutic potential of any drug, researchers use randomized placebo-controlled trials, where some participants receive the drug while others receive a placebo. Ideally, this process is double blinded, meaning neither the participants nor the researchers know who received the drug until the study concludes. The goal is to minimize bias and ensure that any recorded effects are likely due to the drug itself and not participants’ or researchers’ expectations.
But psychedelics make blinding nearly impossible: If you take psilocybin — a hallucinogenic drug that radically alters your subjective experience of reality — you’re unlikely to mistake it for a B vitamin.
Expectation biases — whether in the participants, the researchers, or both — can also complicate psychedelic research. For example, people who agree to participate in studies on drugs like psilocybin, MDMA, or LSD might already have a strong belief that psychedelics can effectively treat mental health conditions.
“This is likely to lead to positive expectation (consciously, subconsciously or both) which is in turn likely to lead to improvements in symptoms after enrollment, regardless of the specific effects of the psychedelics,” noted a 2022 paper published in Psychopharmacology. “This effect also works conversely, in that positive expectations can fuel disappointment in trials of novel psychoactive medication when participants believe that they have been allocated to the placebo arm.”
Still, the results of the recent study are promising, and they add to a growing body of research showing that psilocybin and other psychedelics might possess therapeutic effects that can far outlast the trip experience itself. Considering that 29% of U.S. adults report having been diagnosed with depression at some point in their lives, it’s arguably well worth exploring how psychedelics might help ease the burden of mental health problems.
So far, Oregon and Colorado are the only US states that have legalized psychedelic-assisted therapy, though initiatives in a handful of other states — California, Connecticut, and New Jersey — have aimed to pass similar legislation. Earlier in 2023, Australia became the first country to legalize the prescription of psychedelics, including psilocybin, for mental health conditions.
This article was originally published by our sister site, Freethink.