Aging in human cells successfully reversed in the lab

The ability to reverse aging is something many people would hope to see in their lifetime. This is still a long way from reality, but in our latest experiment, we have reversed the aging of human cells, which could provide the basis for future anti-degeneration drugs.
Aging can be viewed as the progressive decline in bodily function and is linked with most of the common chronic diseases that humans suffer from, such as cancer, diabetes and dementia. There are many reasons why our cells and tissues stop functioning, but a new focus in the biology of aging is the accumulation of “senescent” cells in the tissues and organs.
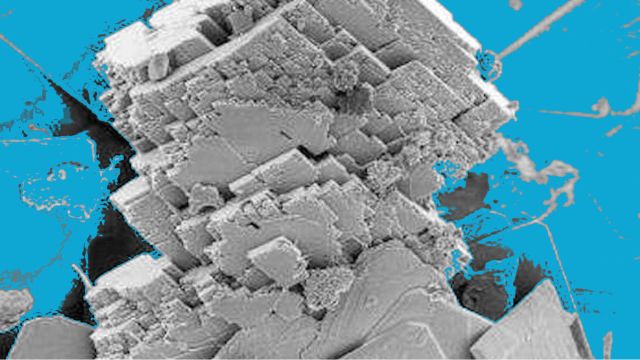
Senescent cells are older deteriorated cells that do not function as they should, but also compromise the function of cells around them. Removal of these old dysfunctional cells has been shown to improve many features of aging in animals such as the delayed onset of cataracts.
We still don’t fully understand why cells become senescent as we age, but damage to DNA, exposure to inflammation and damage to the protective molecules at the end of the chromosomes – the telomeres – have all been suggested.
More recently, people have suggested that one driver of senescence may be loss of our ability to turn genes on and off at the right time and in the right place.
One gene, many messages
As we age, we lose our ability to control how our genes are regulated. Each cell in the body contains all the information needed for life, but not all genes are switched on in all tissues or under all conditions. This is one of the ways that a heart cell is different from a kidney cell, despite the fact they contain the same genes.
When a gene is activated by signals from inside or outside the cell, it makes a molecular message (called an RNA) that contains all the information needed to make whatever that gene makes. We now know that over 95% of our genes can actually make several different types of messages, depending on the needs of the cell.
A good way to think about this is to consider each gene as a recipe. You could make either a vanilla sponge, or a chocolate cake, depending on whether you include the chocolate. Our genes can work like this. The decision as to which type of message is produced at any given time is made by a group of about 300 proteins called “splicing factors”.
As we age, the amount of splicing factors we are able to make declines. This means that aged cells are less able to switch genes on and off to respond to changes in their environment. We and others have shown that the levels of these important regulators decline in blood samples from elderly humans, and also in isolated human senescent cells of different tissue types.
Rejuvenating old cells
We have been looking for ways to turn the splicing factors back on. In our new work, we showed that by treating old cells with a chemical that releases small amounts of hydrogen sulphide, we were able to increase levels of some splicing factors, and to rejuvenate old human cells.
Hydrogen sulphide is a molecule that is found naturally in our bodies and has been shown to improve several features of age-related disease in animals. But it can be toxic in large amounts, so we needed to find a way to deliver it directly to the part of the cell where it is needed.
By using a “molecular postcode” we have been able to deliver the molecule directly to the mitochondria, the structures that produce energy in cells, where we think it acts, allowing us to use tiny doses, which are less likely to cause side effects.
We are hopeful that in using molecular tools such as this, we will be able to eventually remove senescent cells in living people, which may allow us to target multiple age-related diseases at once. This is some way in the future yet, but it’s an exciting start.
Lorna Harries, Associate Professor in Molecular Genetics, University of Exeter and Matt Whiteman, Professor of Experimental Therapeutics, University of Exeter
This article was originally published on The Conversation. Read the original article.