A bizarre facial tumor has decimated the Tasmanian devil population in recent years. Spurred by a worried grad student, Gregory Hannon set out to unlock the secrets of the disease.
Question: What insights did your research reveal into the origins of the facial cancer wiping out Tasmanian devils?
rnGregory Hannon: Well, this is, I think, an interesting story about the social aspects of science in a way. The realization that this transmissible cancer even existed came from a graduate student in my lab who happened to be Tasmanian. She did her PhD on basic aspects of RNA biology, and when she finished her degree before she moved on to a position as a post doctoral fellow, she was looking for a transition project. And she explained to me that this transmissible cancer existed that, in the last 10 years, it had wiped out roughly half of the Devil population and that it was estimated to actually drive the Devils to extinction sometime in the next 30 or so years if nothing were to be done. So, she was very passionate about his and convinced me that we had the tools to try to understand at least something about the biology of this disease.
rnNow, there are only two transmissible cancers that I know about where the cancer itself, the cancer cells themselves move from one individual to another. There’s this Tasmanian Devil facial tumor and there is also a tumor that does this in dogs. In dogs, the tumor isn’t as aggressive. It often spontaneously goes into remission and doesn’t often kill the animals that are, in essence, infected with this. In Tasmanian Devils the tumor is extremely aggressive, often kills affected animals in roughly six months with these horrific facial tumors that ultimately kill the animal often because they grow so large that the animal can no longer eat. But it’s a very aggressive disease also in the sense that it metastasizes to many sites in the body, but the animals are killed so quickly that it’s usually not the metastases that cause them to succumb as happens in many instances of human cancer.
rnSo, our basic question was really to try to understand the origins of this transmissible tumor to try to understand what cell type the tumor was derived from so that we could maybe gain some insight into to why this tumor has such an unusual etiology. And also to try to understand why it is that this tumor can spread from individual to individual, you know, is that such an unusual property?
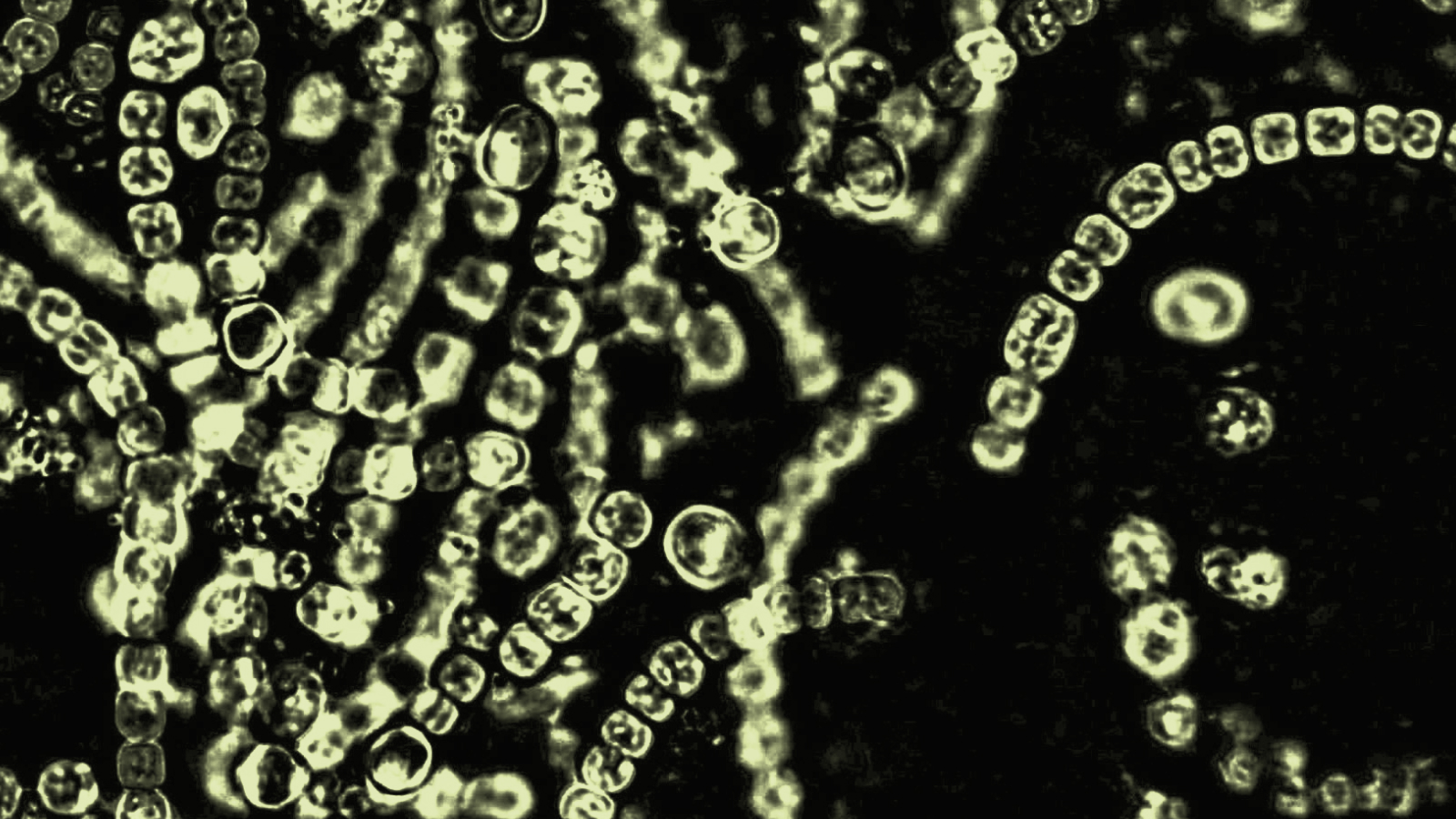
rnWe came at it from a number of different perspectives. First, really founded upon our work on small RNAs, each cell type expresses a specific repertoire of small RNAs that it uses to regulate genes, but that repertoire is also kind of a signature of the cell type that the small RNAs is expressed in. So you can use a small RNA signature to tell a mammary cell from a germ cell. You can tell a nerve cell from a muscle cell. And so we started off by asking what spectrum of small RNAs these Devil facial tumors expressed. And that pointed us, in addition to looking at the messenger RNAs, these RNAs that encode the proteins within that cell by looking at the small RNA profiles and the messenger profiles. That really led us to a specific cell type, which in this case happens to be a Schwann cell.
rnWhat Schwann cells are is essentially like the insulation on a wire. They wrap nerve cells and act essentially as an insulator to make their conductance of signals more efficient.
rnQuestion: What course of treatment or action does this research suggest?
rnGregory Hannon: Well, I mean, I think the two things that really come out of the work that we’ve done looking both at the tumor and the host animals are that the host animals themselves are remarkably genetically homogeneous. And so, one insight that emerged from the study is that the notion that the tumors may be able to spread from animal to animal essentially like a metastasis, but within a population rather than within an organism, in part because the animals can’t recognize these cells as foreign.
rnNow, in terms of a treatment, it’s difficult to envision wild animals undergoing cancer therapy. You can’t really imagine a mobile ICU in the Tasmanian bush. But one thing that one can consider is a prophylactic therapy. And so cancer vaccines have kind of a bad rap in part because they haven’t worked particularly well for humans, but the unusual nature of the Tasmanian Devil tumor and the fact that every tumor is identical, is a very different situation than one has with human cancers where every cancer is different. It is individual not only to the person, but in its genetic composition. And so, in some cases the difficulties in developing cancer vaccines in humans might be related to the heterogeneity of the tumors, whereas when it is precisely the opposite of the situation in Tasmanian Devils.
rnSo, one can really envision two approaches; one is the approach which is being taken, which is to take a set of Devils and set them aside as an insurance population. And so you essentially sequester disease-free Devils with the idea that should the population actually go extinct in the wild, you have animals to reintroduce. Now in that case, we can use the work that we’ve done, which in essence led to a diagnostic marker for this disease, to ensure that any tumors that that insurance population might develop aren’t DFTD.
rnIn the second instance one might imagine trying to develop a vaccine against this particular unusual tumor cell that could potentially be used on wild populations, although you can imagine the challenges that one would face in doing that.
Recorded on February 9, 2010