The surprising success of “honest placebos” in medicine
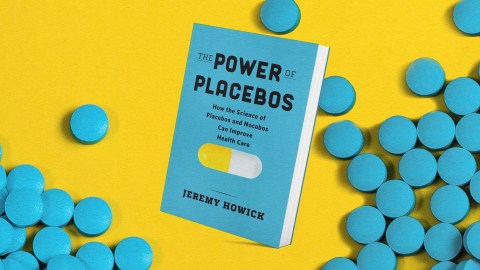
- Lying to patients violates a doctor’s ethical code but happens more often than we might assume — with both placebos and active treatments.
- Placebo treatments do not need to be given deceptively to produce their effects.
- Patients have reported getting better after receiving “honest placebos” — and research is ongoing.
Lying to patients violates part of doctors’ ethical code, which requires them to respect patients’ autonomy. Patients can’t make autonomous decisions if they are being lied to. If I lie and say that a new treatment has no negative side effects, you cannot make an autonomous decision about whether it would be a good idea for you to take it. Sadly, until only a few decades ago, such unethical lying happened more often than we might assume with both placebos and active treatments. [Ethicist and philosopher] Sissela Bok reports a horribly unethical case that might make your blood boil as much as it does mine:
In 1971 a number of Mexican-American women applied to a family-planning clinic for contraceptives. Some of them were given oral contraceptives and others were given placebos, or dummy pills that looked like the real thing. Without knowing it the women were involved in an investigation of the side effects of various contraceptive pills. Those who were given placebos suffered from a predictable side effect: 10 of them became pregnant. Needless to say, the physician in charge did not assume financial responsibility for the babies. Nor did he indicate any concern about having bypassed the “informed consent” that is required in ethical experiments with human beings. He contented himself with the observation that if only the law had permitted it, he could have aborted the pregnant women!
The case Bok describes is horrifying, and experiments like it should be condemned. In 1974, when the essay was published, the kind of lying that Bok describes was not restricted to giving placebo treatments. To name just one example from among too many, the Tuskegee Experiment was a study of Black American men with syphilis between 1932 and 1972. The purpose of the study was to observe what happened to people with syphilis if they were not treated. The men were not treated, though from 1947 onward, they could have been cured with penicillin. The men were not told that treatment was available. The Tuskegee Experiment is a terrible stain on the history of medicine and caused mistrust of the medical profession for decades.
Deception can be unethical even if it helps. In one case, a 14-year-old boy was admitted to the hospital with severe migraines. One of the doctors became concerned about the risk of opioid addiction and substituted morphine with placebo (a saline solution) without the patient knowing. The placebo worked, and the risk of opioid dependence was reduced. This seemed like a good result, but when the mother learned of the deception, she complained. A health care practitioner who was aware of the deception was initially disciplined, although the decision to take disciplinary action was reversed when it was clear that the patient was helped.
In a paper published in 2004 David Wendler and Franklin Miller argued that patients can be deceived if they agree to be deceived. They argue that patients might consent to being deceived without being told what they are being deceived about. Patients might be told something like, “You should be aware that the investigators have intentionally left out information about certain aspects of this study.” I don’t find their argument convincing. To give consent, you must know what you are consenting to. Wendler and Miller respond by noting that patients in these circumstances can only be deceived about matters that would not “affect their willingness to participate.” But how can we know in advance whether something would affect patients’ willingness to participate without asking them first? Their argument seems to rely on an incorrect and paternalistic premise that doctors can guess what might affect patients’ willingness to participate.
Deception is unethical. However, deception is not strictly confined to placebo treatments. The Tuskegee Experiment shows that it also applies to nonplacebo treatments as well. Likewise, it is unethical to withhold a more effective treatment and give a patient a less effective one whether or not the less effective one is a placebo or something else.
Deception is unethical. However, deception is not strictly confined to placebo treatments.
Not only is deception a potential problem with placebo treatments, but placebo treatments do not need to be given deceptively to have their effects — for example the case of Linda Buannono, whose irritable bowel syndrome was cured by honest placebos. In fact, there have been many studies of honest placebos. In the first one I’m aware of, Baltimore doctors Lee Park and Uno Covi gave honest placebos to 15 neurotic patients. They told the patients: “Many people with your kind of condition have been helped by what are sometimes called ‘sugar pills,’ and we feel that a so-called sugar pill may help you too.”
Many of the patients reported getting “quite a bit better” after getting the placebo, even though they knew it was a placebo. The irony of this study is that after getting better, the patients didn’t believe the doctors and thought that the placebos were in fact real drugs (after all, they were neurotic). In a much more recent and rigorous example, 127 patients with chronic back pain (a condition that eats up about 10% of health care budgets in developed nations) were randomized to receive either treatment as usual or honest placebos. They were followed up for three weeks and asked about their pain. Those who received the open-label placebo had less pain than those who received usual treatment. It seems that open-label placebos have effects similar to those of deceptive placebos (placebos that patients think are, or could be, the real treatment). The research on open-label placebos is still growing and it may turn out that they are not as effective as deceptive placebos. Still, we’ve done a systematic review of open-label studies and there is strong evidence that they work, and we know how.