Mortality rates differ by U.S. state. Why?

- After historically being fairly similar, mortality rates now differ by state.
- States that enacted policies to promote healthy habits are now reaping the benefits.
- Moving won’t help, as most of these effects appear to be tied to long-term aspects of health.
Life expectancy in the U.S. declined from a high of 78.8 years in 2019 to 77.3 years in 2020. This is the largest one-year drop since WWII and a reversal of much of the progress made since 2003.
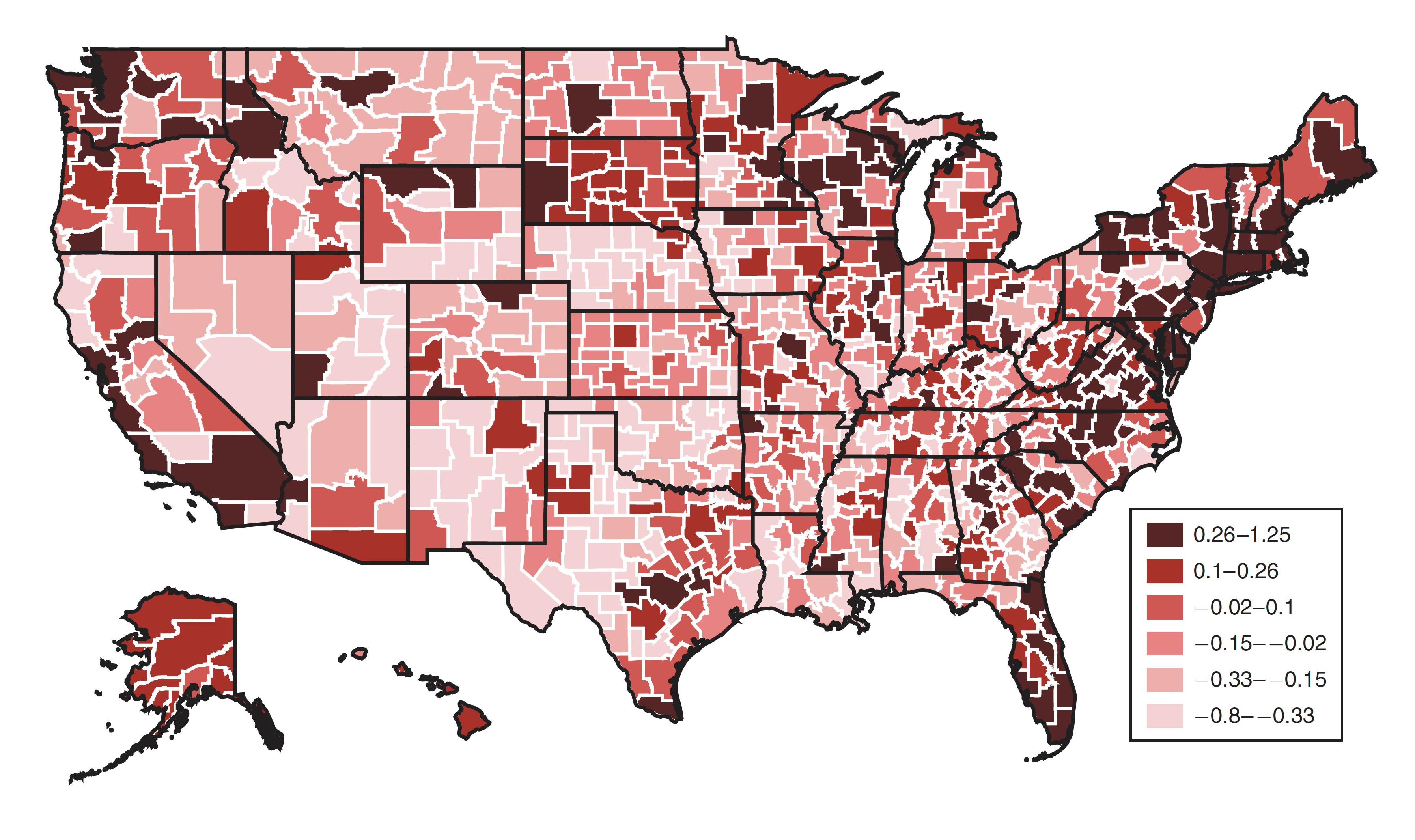
Another alarming development is that mortality rates by state, which used to be similar, have begun to diverge. A new study on this phenomenon, published in the Journal of Economic Perspectives, dismisses easy explanations and instead finds that a broad range of public health issues may be at play.
Mo money, no problems
The mortality (death) rate, which measures the number of deaths in a population over a given period of time (usually a year), used to be fairly similar across the U.S. However, major differences between the states began to appear even before improvements in the national life expectancy leveled out. Indeed, most improvements to longevity after the year 2000 went to the coastal cities while the South and Appalachia stagnated. These differences became more pronounced as the mortality rate for middle-aged Americans increased.
The authors considered a number of possible explanations, focusing first on education and income. As usual, life expectancy goes up with both. But differences between the states on these factors are insufficient to explain the gap in mortality rates. College educated people make up less than a third of the population in most states. And while income very clearly correlates with longevity, the authors indicate that other underlying variables are involved.
Good policy, good health
The authors suggest that the key difference between states is when — if ever — they implemented programs and policies designed to improve public health. As an illustration, the authors compare New York, the state with the fifth lowest overall mortality rate in 2016, with Mississippi, the state with the third highest:
“In New York, for example, smoking rates in 1992 were 22.1 percent, about the same as North Dakota (21.9 percent) and only slightly below Mississippi (23.6 percent). By 2016, smoking had fallen to 9.2 percent in New York, compared to significantly smaller decreases in North Dakota (14.0 percent) and Mississippi (16.6 percent). Since the early 1980s, New York has imposed a substantial excise tax on cigarettes which reached $4.35 per pack in 2016. But as Montez et al. argue, the higher cigarette tax in New York was part of a bundle of initiatives which, to one extent or another, tended to improve public health. For example, New York also participated in Medicaid expansion, implemented its own earned income tax credit, and set a minimum wage above the federal level ($9.00 per hour in 2016). In contrast, Mississippi has a negligible cigarette tax ($0.68 per pack in 2016), opted out of Medicaid expansion, does not offer its own earned income tax credit, and defaulted to the federal minimum wage. In addition, Mississippi has preempted local governments from implementing health-promoting legislation, such as paid sick days, a higher minimum wage, stricter firearm regulations, and nutrition labeling in restaurants.”
So, richer states with a better educated populace tend to enact policies that keep people alive longer. Over the long run, these policy choices lead to a divergence not only in how people live but in how they die.
You can’t cheat death by moving
This study focuses on the long-term impact of living in one place. Other studies have examined the health impact of pulling up stakes and moving to another area. Modest boosts to longevity have been observed for people who move to healthier areas, but the benefits they receive may be unrelated to the health of those already living there. The authors elaborate:
“The cumulative effects of regional policies over the life-cycle — Medicaid coverage at birth, parental income support while a child, tobacco and alcohol taxes during adolescence, and higher-quality medical care during adulthood — are thus likely to exert a larger impact on life expectancy than the short-run impact of moving to a new neighborhood and changing physicians.”
The authors end optimistically, noting that while high-income states have implemented beneficial public health measures first, there is no fundamental reason why lower income states can’t follow suit.